Thymus Gland Cancer
21.03.2025
THYMUS GLAND CANCER DIAGNOSIS AND TREATMENT
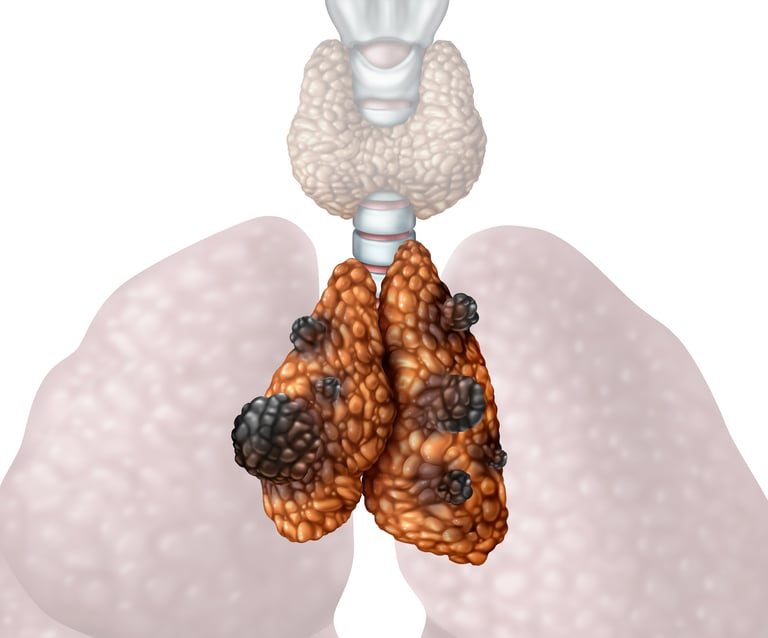
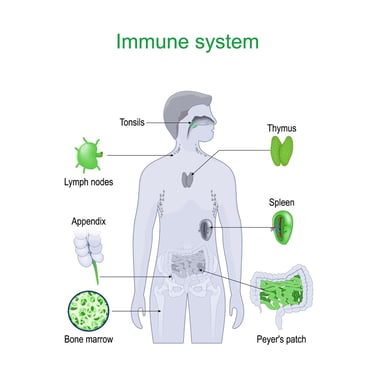
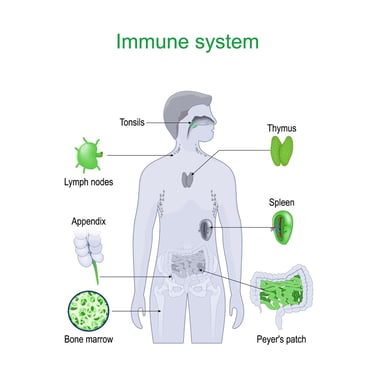
The thymus gland is an organ closely associated with the immune system. The thymus gland is located on the rib cage between the heart and lungs. This gland plays a role in contributing to the maturation of the immune system, being especially active during childhood and adolescence. Thymus helps the development and maturation of white blood cells called T lymphocytes. These cells are the basic components of the immune system that protects the body against diseases and infections.
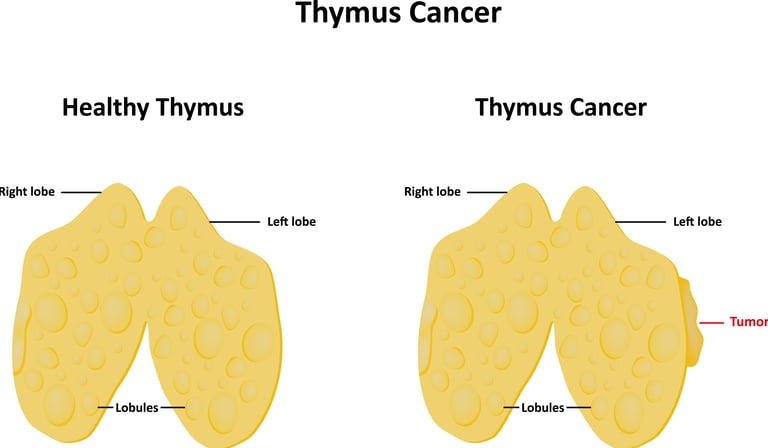
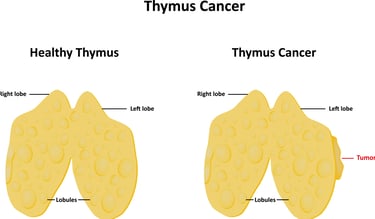
Thymus gland cancer occurs as a result of abnormal cell growth in the thymus gland. This condition is often called thymoma or thymic carcinoma. Thymus gland cancer is generally a rare type, but it can cause certain symptoms, especially chest pain, cough, and shortness of breath.
Although the thymus gland plays an important role in regulating the immune system, thymus gland cancer is a serious condition. Early diagnosis and treatment can increase the chances of success. Therefore, being informed about thymus gland cancer, recognizing its symptoms and regular check-ups can contribute to the early diagnosis of such diseases.
Image 1: The thymus gland is one of the organs in the body that functions in the immune system.
WHAT ARE THE RISK FACTORS?
Although it is not known exactly what causes thymus cancer, certain risk factors may increase the likelihood of developing this type of cancer. However, it should be remembered that these risk factors can only increase a person's likelihood of developing cancer, and many people who develop the disease do not have these risk factors. Potential risk factors for thymus cancer include:
Gender: Thymus cancer is generally more common in young men.
Age: Thymus cancer usually occurs in young and middle-aged adults. However, it can be seen in all age groups.
Genetic Factors: Familial cancer syndromes or genetic mutations may increase the risk of thymus cancer.
Immune System Problems: Immune system problems or long-term use of immunosuppressive medications may increase the risk of thymus cancer.
Other Diseases: Myasthenia gravis may be associated with some other diseases, such as leukemias and autoimmune diseases.
Exposure to Radiation: Radiotherapy, especially to the chest area, may increase the risk of thymus cancer.
Cigarette: Some studies show that smoking may increase the risk of thymus cancer.
Sexually transmitted diseases: Some sexually transmitted viruses, such as human T-lymphotropic virus type 1 (HTLV-1), may increase the risk of thymus cancer.
Although these factors increase the likelihood of developing thymus cancer, just because an individual has these factors does not necessarily mean they will develop this cancer. For rare conditions such as thymus cancer, it can be difficult to pinpoint a definitive cause. Therefore, it is important to consult a healthcare professional with any symptoms or concerns.
HOW DOES IT OCCUR?
Although the development mechanisms of thymus cancer are not fully understood, various studies are being carried out on this subject. Thymus cancer can generally occur as a result of the interaction of genetic mutations, immune system disorders and various environmental factors. Genetic predisposition, familial cancer syndromes, or certain genetic mutations may lead to abnormal growth of thymus cells, contributing to the development of cancer. Immune system problems can pave the way for cancer development, especially in the thymus, which plays a role in the maturation and regulation of T lymphocytes. Exposure to radiation or some viral infections may also increase the risk of thymus cancer. However, these mechanisms are not fully understood, and the factors affecting the development of thymic cancer remain complex.
WHAT ARE THE SYMPTOMS?
Symptoms of thymus cancer may often not be obvious and the disease can often be found incidentally. However, some symptoms that may occur when thymus cancer develops are:
Chest Pain: Because the thymus gland is located in the upper part of the ribcage, a symptom that occurs as cancer develops may be chest pain.
Cough and Shortness of Breath: Thymus cancer can put pressure on the lungs, causing cough and shortness of breath.
Neck Swelling: Thymus cancer can sometimes cause the lymph nodes in the neck to swell.
Weakness and Fatigue: Cancer can deplete the body's energy, causing general weakness and fatigue.
Dry Mouth and Frequent Urination: Thymus cancer can sometimes affect hormones such as parathyroid hormone, which can cause symptoms such as dry mouth and frequent urination.
Myasthenia Gravis: Thymus cancer can sometimes trigger a neuromuscular disorder called myasthenia gravis. This can cause muscle weakness and fatigue.
These symptoms may be signs of another health problem, but it is important to consult a physician, especially if several occur together or persist consistently. In case of any suspicious symptoms, it is important to consult a doctor and undergo the necessary tests. It should not be forgotten that thymus cancer is a rare condition, but it is possible to increase the chance of success with early diagnosis and treatment.
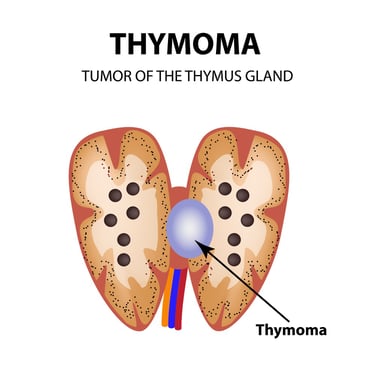
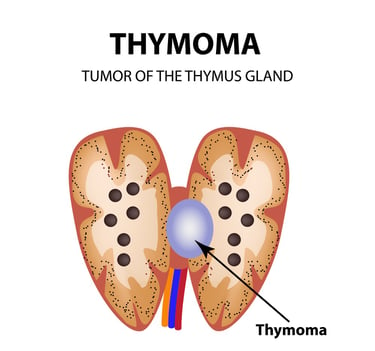
Image 2: Thymomas are generally benign tumors that develop in the thymus gland.
HOW IS IT DIAGNOSED?
Thymus cancer is usually diagnosed using various medical tests and imaging methods. In the diagnostic process, which begins by evaluating the patient's symptoms and medical history, imaging methods such as blood tests, computerized tomography (CT) scans, magnetic resonance imaging (MRI) and positron emission tomography (PET) are generally used. These tests try to identify abnormalities, tumors and other possible problems in the thymus area. Biopsy involves taking a tissue sample and performing laboratory examination, which is important to confirm the presence of cancer cells and determine the type of cancer. The diagnosis of thymus cancer is made as a result of a comprehensive evaluation by a specialist oncologist, and an appropriate treatment plan is created by taking into account the patient's general health condition, medical history and other factors.
WHAT ARE THE PATHOLOGICAL TYPES?
The receptors to be examined in thymus cancer are important to understand the nature of the disease, determine treatment strategies and evaluate prognosis. T-lymphocyte receptors (TCR) play a critical role in determining the type of thymic cancer because these receptors control the development of T lymphocytes. PD-L1 (Programmed Cell Death Ligand 1) is one of the immune checkpoints, and whether thymus cancer cells carry this ligand is important in determining a potential target for immunotherapy treatment. Cell surface markers such as CD5 and CD117 are used in the diagnosis of thymus cancer types such as thymoma and thymic carcinoma. While Ki-67 is used to assess the level of cellular proliferation, tyrosine kinase receptors (e.g., EGFR, c-Kit) and hormone receptors are important for understanding the biological characteristics of thymic cancer and developing specific treatment strategies. Evaluation of these receptors helps personalize the patient's treatment plan and determine the most effective approach.
Thymus tumor may include different subtypes according to their pathological type.
Thymus Hyperplasia: Thymus hyperplasia means more cell growth than normal in the thymus gland. This condition is usually benign and not cancerous, but it can affect the normal function of the thymus.
Timoma: Thymoma is a type that originates from the thymus tissue and is typically benign (non-invasive). However, in some cases it may contain cancerous cells. If the thymoma has cancerous cells, the condition may be called thymic carcinoma.
Thymic Cancer: Thymic carcinoma is a type of cancer that originates from thymus cells. Thymic carcinoma can often be more aggressive and tends to spread (metastasize) to other tissues.
Lymphoma: Thymus lymphoma is a type of cancer that arises from the lymphocytes of the thymus.
Thymus cancer may have one or more of these pathological types. Each type can affect the nature of the cancer, treatment approaches, and prognosis. The diagnosis of the patient is made based on the results of pathological examination, which is usually obtained by examining the tissues taken during biopsy under a microscope.
HOW IS TUMOR STAGING DONE?
Staging of thymus cancer is the process of determining the extent of spread of the disease and is important in creating a treatment plan. Thymus cancer staging is usually based on the following factors:
Tumor Size (T): It determines the size of the thymus cancer tumor and whether it is limited to the thymus gland. This is generally divided into categories such as T1, T2, T3 and T4, increasing in stage as size increases.
Lymph Node Status (N): It is important to evaluate the spread to lymph nodes in the staging of thymus cancer. If there is spread to lymph nodes, the stage increases. This is usually divided into categories such as N0, N1, N2.
Distant Organ Metastases (M): Thymus cancer can metastasize to other organs. To determine this situation, the presence or absence of metastasis in distant organs is evaluated. In case of distant metastasis, it is the last stage.
By combining this information, a staging system based on the "TNM" system is often used. Thymus cancer stages are generally classified as I, II, III and IV, with stage IV representing the last stage. During the staging process, imaging methods, technologies such as computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) are also used. These imaging methods can help evaluate tumor size, spread to lymph nodes, and distant organ metastases in more detail. Thymus cancer staging is important to determine the extent of disease spread and determine appropriate treatment strategies. This staging process helps to better understand the prognosis of the disease and response to treatment.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Treatment for thymus cancer is individualized according to the stage and type of disease, the patient's general health status, and other individual factors.
Stage I and II: In these stages, the tumor is usually limited to the thymus gland. Surgical intervention (removal or partial removal of the thymus gland) is frequently preferred in these stages. Surgical intervention aims to prevent the spread of the tumor to surrounding tissues and to control the disease.
Stage III: Thymus cancer may have spread to surrounding lymph nodes at this stage. In addition to surgery, treatment methods such as radiotherapy (destroying cancer cells using high-energy rays) and chemotherapy (killing cancer cells using drugs) can be used in combination.
Stage IV: At this stage, thymus cancer may have metastasized to other parts of the body. Treatment may often include a combination of surgery, radiotherapy and chemotherapy. Additionally, new treatment options such as targeted therapy and immunotherapy may also be considered.
The treatment plan is determined by a multidisciplinary healthcare team and is customized based on factors such as the patient's general health condition, age, and biological characteristics of the disease. The patient's response to treatment is important in the management of the treatment process. Every patient is different, so the treatment plan should be evaluated individually. During the treatment process, patients should cooperate with healthcare professionals and obtain detailed information about treatment options.
Image 3: Thymus gland cancer is a rare malignant tumor of the thymus gland.
WHAT ARE THE DRUGS USED IN TREATMENT
Chemotherapy, hormonal drugs, smart drug treatments and immunotherapies used in the treatment of thymus cancer may vary depending on the patient's specific condition, type and stage of cancer. However, some commonly used medications and treatment approaches are:
Chemotherapy drugs:
Cisplatin: It is a platinum-based chemotherapy drug frequently used in the treatment of thymus cancer.
Doxorubicin: It is an antitumor drug that targets cancer cells and prevents them from multiplying.
Etoposide: It is a drug that stops cell division and can be used in the treatment of thymus cancer.
Carboplatin: It is another platinum-based chemotherapy drug and may be effective against thymus cancer.
Smart Drug Therapies:
Tyrosine Kinase Inhibitors: Drugs that target tyrosine kinase receptors such as EGFR (Epidermal Growth Factor Receptor) or c-Kit (sunitinib, lenvatinib) can be used in the treatment of thymus cancer.
Immunotherapies:
PD-1 or PD-L1 Inhibitors: Immunotherapy drugs such as pembrolizumab and nivolumab can be used in the treatment of thymus cancer by stimulating the immune system.
Every patient is different and the treatment plan is shaped according to individual characteristics. Treatment options are determined depending on the patient's general health, the stage and type of disease, and other factors. The treatment process is guided by a medical oncologist and the patient's response to treatment is evaluated regularly.
HOW SHOULD FOLLOW-UP BE DONE AFTER RECOVERY?
Monitoring patients after thymus cancer treatment is important for early detection of disease recurrence or other problems. Post-recovery follow-up usually includes regular check-ups. These check-ups are usually managed by an oncologist and are planned taking into account the patient's general health condition, response to treatment, side effects and quality of life. Follow-up exams may include imaging tests (such as CT, MRI, PET), blood tests, and physical exams. These checks are organized to closely monitor the patient's health and, if necessary, re-evaluate the treatment plan. Additionally, the psychosocial effects of the disease and lifestyle factors are also evaluated. A good follow-up plan plays an important role in maintaining the patient's health in the best possible way and managing the process of fighting the disease.