How is Cancer Diagnosed?
21.03.2025
HOW IS CANCER DIAGNOSED?
The process of diagnosing cancer usually begins when suspicious symptoms or abnormal results on screening tests occur. During the cancer diagnosis process, the physician makes a preliminary evaluation based on physical examination and symptoms. More detailed tests are then applied. These tests often include blood tests, imaging methods (e.g., X-ray, CT, MRI, PET scans), and most importantly, pathological examination of biopsy samples taken from suspicious tissue. Biopsy is the gold standard for confirming the presence, type, and other important characteristics of cancer cells. Sometimes additional tests, such as genetic testing or tumor markers, are also used to better understand the type of cancer and determine treatment options. The diagnostic process varies depending on the type of cancer and the individual situation of the patient and often requires a multidisciplinary approach. This gradual and comprehensive process helps determine the most appropriate treatment method and increases the success of cancer treatment.
Stages of the process of diagnosing cancer:
1-Examination of Symptoms and Physical Examination: The patient tells the doctor about his symptoms. These symptoms may include weight loss, fatigue, pain, or the sensation of tumors. The doctor physically examines the patient and checks for any abnormalities (for example, a swelling or mass).
2-Review of Medical History: The doctor reviews the patient's personal and family medical history. This examination is important to evaluate cancer risk.
3-Laboratory Tests: Blood tests and tests of other body fluids can show signs of cancer. For example, some types of cancer can cause changes in blood cells. Tumor markers are substances that can indicate the presence of cancer in the body and are generally produced by cancer cells or increased in the presence of cancer. These can be found in blood, urine or tissues and can provide important information for diagnosing cancer, planning treatment and monitoring the disease.
The use of tumor markers may be for the following purposes:
Diagnosis: Some tumor markers may be helpful in the early diagnosis of certain types of cancer. However, most tumor markers are nonspecific and cannot be used to diagnose cancer. They are often evaluated together with other diagnostic methods.
Prognostic Information: Some tumor markers can be used to predict the stage of cancer and its prognosis (course of the disease).
Monitoring Response to Treatment: Changes in tumor marker levels during and after treatment may be an indicator of the effectiveness of the treatment. Decreasing marker levels may indicate that the treatment is successful, while increasing levels may indicate recurrence or progression of the disease.
Follow-up of the disease: In the post-treatment period, regular monitoring of tumor marker levels may help detect cancer recurrence at an early stage.
Examples of some common tumor markers:
CA-125: Commonly used in the follow-up of ovarian cancer.
PSA (Prostate Specific Antigen): Used in the diagnosis and follow-up of prostate cancer.
CEA (Carcinoembryonic Antigen): It is used in the follow-up of colorectal and some other types of cancer.
Tumor markers are an important tool in diagnosing and monitoring cancer, but they often need to be evaluated in conjunction with other diagnostic methods because many tumor markers can be elevated in non-cancerous conditions and there is no specific tumor marker for every type of cancer. Therefore, it is important to consult an experienced healthcare professional regarding the interpretation of tumor marker results.
Image 1: Imaging methods such as CT, MRI, USG and PET can be used to detect the location and spread of cancer.
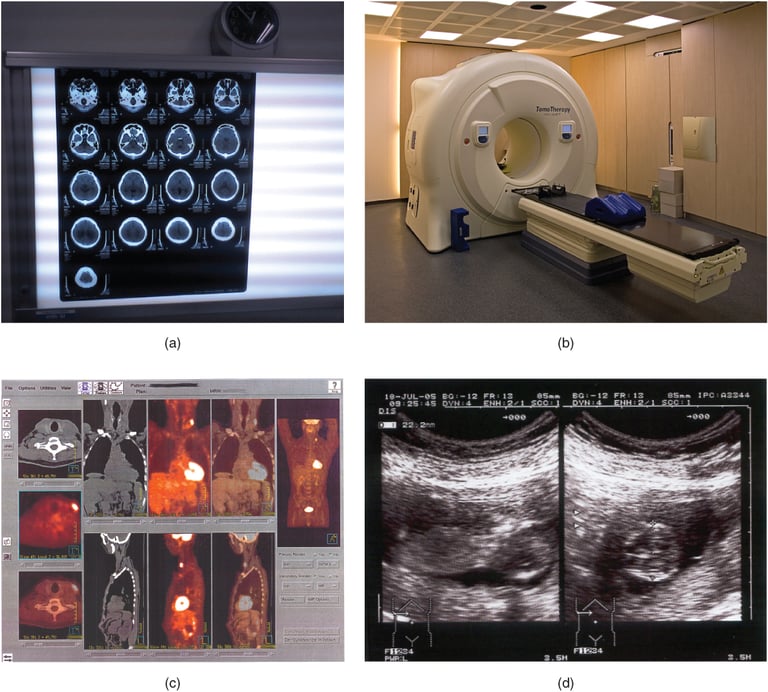
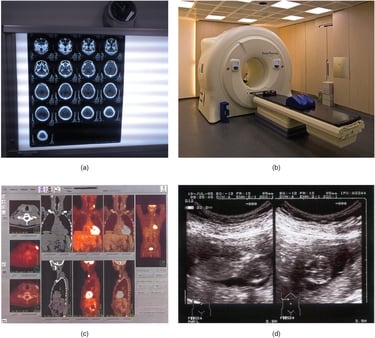
4-Imaging Tests: X-ray, CT, MRI and Positron Emission Tomography (PET) Imaging tests provide detailed images of the inside of the body. These tests may show abnormal tissues or changes in organs.Not every cancer patient needs to have a PET scan. PET is an important imaging method used especially in staging cancer, investigating metastasis (spread of cancer to other organs) and evaluating response to treatment. However, the use of a PET scan varies depending on the type of cancer, its stage, the patient's overall health and treatment plan. A PET scan is not a standard procedure for all types of cancer and may not be necessary for every patient. Doctors recommend a PET scan based on the patient's needs and specific condition. Other imaging methods (CT, MRI, etc.) and tests such as biopsy are also commonly used in cancer diagnosis and follow-up. Therefore, the necessity of a PET scan should be determined by the physician based on each patient's individual situation.
5-Biopsy: A small piece of suspicious tissue is taken and examined in the laboratory. This is the most accurate method to confirm the presence and type of cancer. Biopsy for the diagnosis of cancer is performed by taking a sample of suspicious tissue and microscopic examination of these samples in the laboratory. The biopsy method varies depending on the location and size of the tumor. The most common methods can be classified as needle biopsy (fine needle aspiration or core biopsy), excisional and incisional biopsy. Needle biopsy involves taking a tissue sample from the tumor using a thin or thick needle, usually under local anesthesia, and is a minimally invasive method. Excisional biopsy involves surgically removing all of the suspicious tissue, while incisional biopsy involves removing only a portion of it. The tissue samples taken are examined in detail in the laboratory to determine the presence, type and other pathological features of cancer cells. Biopsy is one of the most reliable methods in diagnosing cancer and is of critical importance in diagnosis, treatment planning and prognosis determination. This procedure is usually performed under the guidance of radiological imaging techniques (such as ultrasonography, CT, or MRI), which allows better identification of the correct area to sample.
6-Pathological Examination: The tissue sample taken during the biopsy is examined under a microscope to determine the presence and type of cancer cells. Pathological examination is the microscopic examination of tumor tissue taken by biopsy or surgery in a laboratory environment. In this process, pathologists determine the presence, type, degree of aggressiveness and other important characteristics of cancer cells by staining tissue samples and applying special tests. Pathological examination is critical for the definitive diagnosis of cancer, and the results of this analysis provide basic information for determining the stage of cancer, selecting the appropriate treatment method, and predicting the prognosis (possible course of the disease). In particular, it provides detailed information about cancer by examining the cellular structure of the tumor, its spread and its relationship with neighboring tissues. Therefore, pathological examination is an integral part of the cancer diagnosis and treatment process.
7-Genetic Tests: Genetic testing can be done for some types of cancer. These tests are important to understand whether the cancer is hereditary.The importance of genetic tests in cancer diagnosis is increasing. These tests analyze genetic changes, mutations, and other genetic factors in cancer cells. This information is used to better understand the type and subtype of cancer, personalize treatment options, and determine the most appropriate treatment methods for the patient. Particularly in some types of cancer, the effectiveness of new treatment methods such as targeted therapies and immunotherapy may depend on certain genetic characteristics. Genetic testing can also be used to understand whether cancer is inherited in families and to develop early diagnosis and preventive strategies for family members at risk. The use of genetic tests contributes greatly to making cancer treatment more effective and personalized and becomes an important part of personalized medicine. Therefore, genetic testing is becoming increasingly important in modern cancer diagnosis and treatment approaches.
Image 2. The definitive diagnosis of cancer is made by examining the biopsy piece under a microscope in the pathology department.


8-Post-Diagnosis Evaluation and staging: Once cancer is diagnosed, the stage and spread of the disease are determined. This is an important factor in creating a treatment plan. Determining the stage of cancer is vital to understanding how far the cancer has spread in the body and plays a fundamental role in treatment planning. This process is usually done using the TNM classification system, taking into account the size and spread of the tumor (T), spread to nearby lymph nodes (N), and metastasis to other organs (M). The size and local extent of the tumor are evaluated by physical examination, biopsy, and various imaging tests (e.g., MRI, CT, PET scans). Similar tests are used to determine spread to lymph nodes and other organs. In some cases, the stage can be determined more clearly by pathological examination of samples taken during surgery. The stage of cancer is critical for understanding the prognosis (likely course) of the disease, determining treatment options, and evaluating treatment response. Staging criteria may differ for each type of cancer and the process is based on detailed clinical guidelines specific to the cancer type.
9-Treatment Planning: Depending on the cancer type and stage, treatment options such as surgery, radiotherapy, chemotherapy, immunotherapy or targeted therapy are evaluated. Cancer treatment planning is done with a multidisciplinary approach, taking into account the patient's cancer type, stage, general health status and personal preferences. This process is carried out by a team of oncologists, surgeons, radiation therapists, pathologists and other healthcare professionals. First of all, the type and spread of cancer are determined by detailed medical tests (biopsy, imaging tests, genetic tests, etc.). Then, depending on the characteristics of the cancer and the patient's health condition, various treatment options such as surgery, chemotherapy, radiotherapy, immunotherapy or targeted therapies are evaluated. The patient's lifestyle, tolerance to treatment and personal preferences also play an important role in treatment planning. Treatment options are carefully balanced taking into account potential side effects, treatment effectiveness, and the patient's quality of life. Ongoing monitoring and evaluation are part of the treatment process so that treatment can be adjusted as necessary and optimized for the patient's needs. This comprehensive and personalized approach aims to increase the success of cancer treatment and support the patient's overall health and well-being.
The process of diagnosing cancer can vary from person to person and may involve different tests and procedures depending on the specific type of cancer. The most important step in this process is to determine the most accurate and effective treatment methods suitable for the patient's condition.