Immunotherapy
21.03.2025
IMMUNOTHERAPY DRUGS IN CANCER TREATMENT
Immunotherapy is an innovative treatment method used in the treatment of various diseases, including cancer. This treatment helps the patient fight the disease by strengthening his own immune system. In cancer treatment, immunotherapy activates and strengthens the immune system, which normally cannot recognize and destroy cancer cells. This can be done by developing antibodies to specific proteins on the surface of cancer cells or by making immune cells more effective against cancer cells. The advantages of immunotherapy include that it is a targeted treatment and that its side effects are different and sometimes less than traditional treatments. Additionally, immunotherapy can, in some cases, promote a long-lasting immune response against cancer cells, which may reduce the risk of cancer recurrence. Immunotherapy has been particularly effective in cancer types such as melanoma, lung cancer, and some lymphomas and is considered a significant advance in cancer treatment.
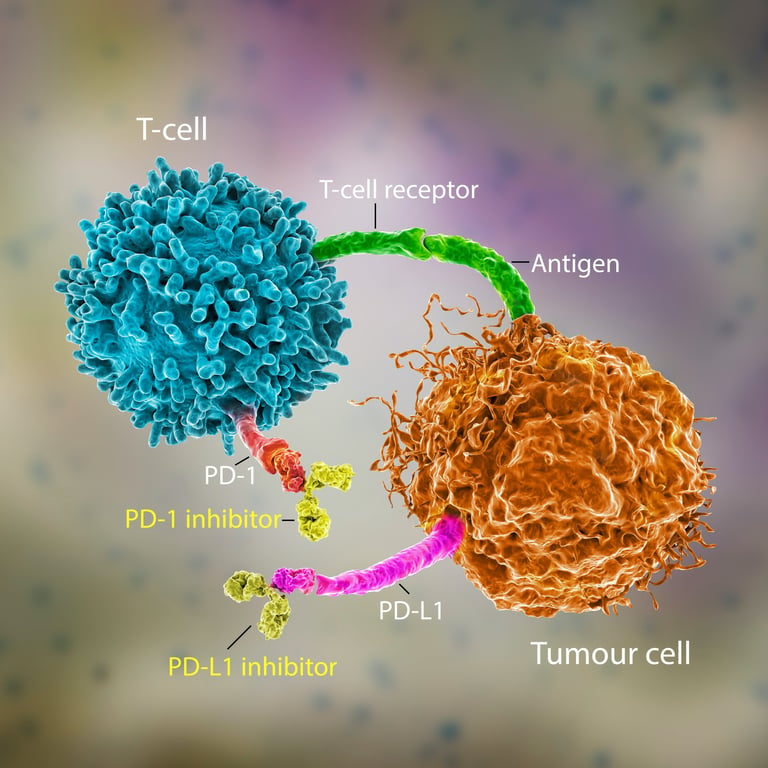
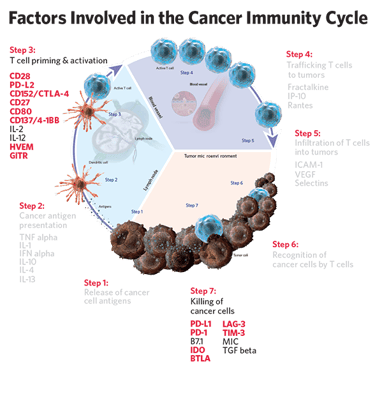
Image 1: There are many different cells and molecules involved in the immune system.
WHAT ARE THE TYPES OF IMMUNOTHERAPY TREATMENTS?
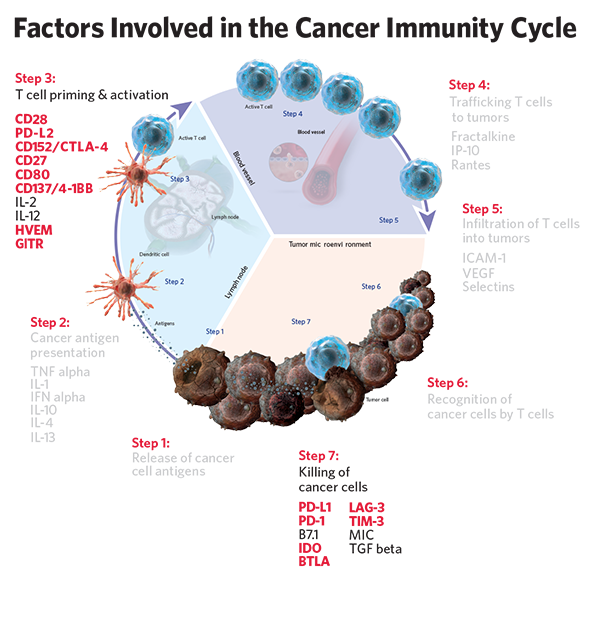
Immunotherapy is the general name of treatment methods that aim to combat diseases such as cancer by activating the immune system. These treatments help the immune system recognize and destroy cancer cells. The various types of immunotherapy treatments are detailed below:
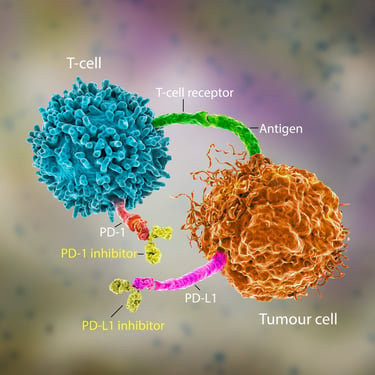
Immune Checkpoint Inhibitors: These drugs target proteins (checkpoints) that allow cancer cells to escape the immune system. Checkpoint inhibitors activate the immune system more effectively against cancer cells by blocking proteins such as PD-1, PD-L1 and CTLA-4. Examples of these drugs include pembrolizumab (PD-1 inhibitor), nivolumab (PD-1 inhibitor), and ipilimumab (CTLA-4 inhibitor).
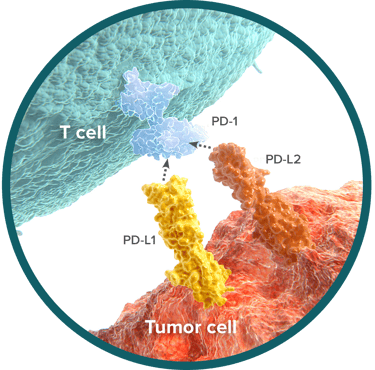
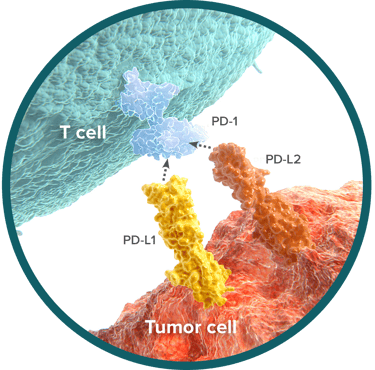
Blockade of the PD-1/PD-L1 Pathway: Programmed cell death protein 1 (PD-1) and its ligand PD-L1 are a checkpoint that suppresses the activity of T-cells. Cancer cells can evade the immune system by having PD-L1 on their surface. PD-1 or PD-L1 inhibitors block this interaction, allowing T-cells to attack cancer cells.
PD-1 Inhibitors:
Pembrolizumab: Approved for many types of cancer, including melanoma, non-small cell lung cancer (NSCLC), and head and neck squamous cell carcinoma.
Nivolumab: Used to treat melanoma, NSCLC, renal cell carcinoma, Hodgkin lymphoma, and bladder cancer.
PD-L1 Inhibitors:
Atezolizumab: Used in the treatment of urothelial carcinoma and NSCLC.
Durvalumab: It is used especially in the treatment of non-small cell lung cancer and bladder cancer.
CTLA-4 Pathway Blockade: Cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) is also a checkpoint and regulates the immune response by suppressing T-cell activation. CTLA-4 inhibitors block the suppressive effect of this protein on the immune system, which allows T-cells to develop a more effective response against cancer cells.
Ipilimumab: First approved for use in the treatment of metastatic melanoma. It increases T-cell activation by targeting CTLA-4.
Checkpoint inhibitors are considered a significant advance in cancer treatment and have been proven effective in various types of cancer. However, these drugs have specific side effects and may not be suitable for every patient. Therefore, the choice of treatment options and medications should be evaluated on an individual basis, taking into account the patient's general health status and the type of cancer.
Cancer Vaccines: Cancer vaccines are specifically designed to stimulate the body's immune response against cancer cells. These vaccines contain specific antigens usually found on the surface of cancer cells and enable the immune system to launch an attack against these cells. For example, sipuleucel-T is a cancer vaccine used to treat metastatic prostate cancer.
Adoptive Cell Transfer (ACT): This method involves taking the patient's own immune cells, genetically modifying and strengthening them in the laboratory, and injecting them back into the patient's body. CAR T-cell therapy is the most well-known example of this method and is used especially in the treatment of some blood cancers. In this treatment, T-cells are modified to recognize antigens specific to cancer cells and then returned to the patient.
Monoclonal Antibodies: These drugs can stop the growth of cancer cells or destroy them by binding to specific proteins on the surface of cancer cells. Some monoclonal antibodies also function as immune checkpoint inhibitors. Examples are rituximab (for B-cell lymphomas) and trastuzumab (for HER2-positive breast cancer).
Oncolytic Virus Treatment: This treatment uses genetically modified viruses to infect and destroy cancer cells. While these viruses target cancer cells, they cause less harm to normal cells and may also help the immune system mount a response against cancer cells.
Cytokine Therapy: Cytokines are proteins that immune system cells use to communicate. In this treatment, the response of the immune system is strengthened by using cytokines such as interferons and interleukins. For example, interferon-alpha is used in some types of cancer and melanoma.
Immunotherapy treatments are customized based on the type and stage of cancer and the patient's overall health and are often used in combination with other treatment methods. These treatments are considered an important innovation in cancer treatment and offer new treatment options as a constantly developing field.
Image 2: Immunotherapies neutralize the mechanisms that prevent cancer cells from escaping the immune system.
WHAT ARE THE ADVANTAGES?
Immunotherapy has some important advantages in cancer treatment over other standard treatments (chemotherapy, radiotherapy, surgery). These benefits include:
Targeted Therapy: Immunotherapy is often more specifically targeted at cancer cells. This reduces the risk of damage to healthy cells and side effects may be different than traditional treatments.
Longer Lasting Response: Immunotherapy can provide long-term remission in some patients. The immune system "remembers" cancer cells and can quickly destroy them when they appear again.
Less Side Effects: The side effects of immunotherapy are generally less severe and of a different nature than the side effects caused by chemotherapy or radiotherapy. This may make the treatment process more tolerable for patients.
Effectiveness in Metastatic Cancers: Immunotherapy can be effective, especially in metastatic or advanced-stage cancers, when other treatment methods are inadequate.
Personalized Treatment: Immunotherapy can be customized based on the characteristics of the patient's immune system and cancer, allowing for personalized treatment approaches.
Decreased Development of Resistance Against Cancer Cells: Cancer cells that develop resistance to conventional treatments may be less resistant to immunotherapy. This increases the effectiveness of the treatment.
Combined Treatment Possibilities: Immunotherapy may show synergistic effects when combined with other cancer treatments (chemotherapy, targeted therapies, radiotherapy), which may increase treatment effectiveness.
These advantages indicate that immunotherapy plays an important role in cancer treatment and will occupy a central place in future cancer treatment strategies. However, immunotherapy also has specific side effects and limitations and may not be suitable for every patient. Therefore, determining treatment options should be evaluated individually based on factors such as the patient's general health condition, cancer type and stage.
IN WHICH CANCERS IS IT EFFECTIVE?
Although immunotherapy is a revolutionary approach to cancer treatment, it does not respond equally effectively to all types of cancer. Some types of cancer are particularly sensitive to immunotherapy, while others may be less responsive or unresponsive.
Cancers Sensitive to Immunotherapy
Melanoma: It is one of the types of cancer for which immunotherapy is most effective. Particularly PD-1 and CTLA-4 inhibitors have shown significant success in the treatment of melanoma.
Non-Small Cell Lung Cancer:PD-1 and PD-L1 inhibitors may be effective in this type of cancer.
Renal Cell Carcinoma: Immunotherapy is especially used in the treatment of advanced stage kidney cancer.
Head and Neck Cancers: Some advanced head and neck cancers respond well to immunotherapy.
Hodgkin Lymphoma: PD-1 inhibitors, in particular, can be effective in this type of cancer.
Bladder Cancer: Immunotherapy is used to treat advanced bladder cancer and may be effective in some patients.
Cancers Unresponsive to Immunotherapy
Pancreas Cancer: Generally unresponsive to immunotherapy, this type of cancer has effective mechanisms to evade the immune system.
Glioblastoma: Brain tumors often create a microenvironment that is protective against the immune system, which reduces the effectiveness of immunotherapy.
Prostate cancer: The effectiveness of immunotherapy may be limited in this type of cancer, but immunotherapy may be used in some specific cases.
Ovarian Cancer:This type of cancer is generally less responsive to immunotherapy.
Colon Cancer (Microsatellite Instability): CNS colon cancer is generally unresponsive to immunotherapy, but colon cancers with high microsatellite instability (MSI-H) may be more sensitive.
These generalizations illustrate the complex nature of immunotherapy and the importance of individual differences in cancer treatment. The effectiveness of immunotherapy in cancer treatment depends on many factors, such as the molecular characteristics of the cancer, its microenvironment, and the general health status of the patient. Therefore, treatment options and strategies must be customized for each patient.
Image 3: Immunotherapies can be used in cancer treatment in all cancer patients whose markers such as MSI, PD-L1, TMB are positive or at appropriate levels.
THE WAY, FREQUENCY AND DURATION OF APPLICATION OF MEDICATIONS
The use of immunotherapy drugs may vary depending on the type of drug and the type of cancer to be treated. Immunotherapy drugs are usually administered by:
Intravenous (IV) Administration: The most common immunotherapy application is the intravenous route. The medication is administered directly into the bloodstream through a vein. This practice is usually performed by oncology physicians and nurses in a hospital or a treatment center. Treatment may be repeated at regular intervals (for example, every 2-3 weeks).
Treatment Protocols: The frequency and duration of administration of immunotherapy drugs vary depending on the type of cancer, the type of drug, and the patient's response to treatment. Some treatment protocols call for medication to be given once a week or less frequently.
Treatment Duration: Treatment duration is variable and can sometimes last from several months to several years. Depending on the patient's condition and response to treatment, the duration of treatment can be adjusted.
The use of immunotherapy drugs has an important role in cancer treatment, and the administration of these drugs should be customized to the individual needs of each patient. During the treatment process, it is important for patients to maintain close communication with their doctor and healthcare team and report any side effects immediately.
SIDE EFFECTS OF IMMUNOTHERAPY DRUGS
Immunotherapy drugs are powerful drugs used to treat cancer and work by modulating the immune system. The side effects of these drugs usually arise from the immune system and are different from the side effects of traditional chemotherapy drugs.
Side effects: Side effects of immunotherapy drugs are often different from the side effects of traditional chemotherapy and may depend on the immune system. Side effects may include skin reactions, fatigue, diarrhea, liver dysfunction, and more serious autoimmune reactions.
Regular Monitoring: During immunotherapy, patients are monitored regularly. It may include blood tests, imaging tests, and physical exams. This monitoring is critical for managing side effects and assessing response to treatment.
Listed below are some common side effects of immunotherapy medications and treatments for these side effects:
Tiredness: It is one of the most common side effects and can be seen in the majority of patients.
Skin Reactions: Skin reactions such as redness, itching and rash are common.
Digestive System Problems: Digestive system problems such as diarrhea, abdominal pain and colitis (inflammation of the intestine) may occur.
Lung Problems: Lung problems such as pneumonitis may occur. This condition is characterized by inflammation of the lung tissue.
Endocrine System Effects: Endocrine system effects such as thyroid gland dysfunction, hypophysitis (inflammation of the pituitary gland) and type 1 diabetes may develop.
Liver Function Disorders: Liver problems such as elevation of liver enzymes and hepatitis may occur.
Autoimmune Reactions: Immunotherapy can cause autoimmune reactions (the body attacks its own tissues) in some patients.
TREATMENT METHODS OF SIDE EFFECTS
Supportive Treatments: Supportive treatments for fatigue and skin reactions can be applied, for example skin creams or activity modifications to reduce fatigue.
Drug Treatments: For digestive problems, anti-diarrheal medications or anti-inflammatory medications may be prescribed.
Corticosteroids: For serious inflammatory side effects (such as pneumonitis or colitis) corticosteroids may be used.
Treatment Interruption or Adjustment: In case of serious side effects, the immunotherapy dose may need to be reduced or treatment temporarily stopped.
Hormone Replacement Therapies: Hormone replacement therapies may be administered for endocrine system effects, such as problems with the thyroid or adrenal glands.
Special Drug Treatments: Special drug treatments may be required for some autoimmune reactions or liver dysfunction.
Management of side effects should be evaluated individually for each patient. It is important for patients to report side effects to their doctors and to stay in close communication with their treatment team. Regular medical monitoring during immunotherapy is critical for early detection and effective management of side effects. Side effects can usually be controlled by discontinuing the medication or adjusting the dose, but in some cases more aggressive medical intervention may be required.
CONCLUSION
Immunotherapy is considered one of the most revolutionary advances in cancer treatment and this treatment method has opened a new horizon in the fight against cancer. Essentially, immunotherapy works by using the body's own immune system against cancer cells. This approach has been a great source of hope, especially in cases where traditional treatments are ineffective or in advanced stages of cancer. Immunotherapy has the advantage of causing minimal damage to healthy cells by specifically targeting cancer cells, which may reduce the severity of side effects. The long-term remissions it provides in some patients indicate the beginning of a new era in cancer treatment. The personalized treatment options offered by immunotherapy have enabled us to better understand the complexity of cancer biology and enable the development of more targeted, effective treatment strategies for patients. This success of immunotherapy emphasizes the importance of innovative approaches in cancer research and paves the way for the discovery of more effective methods in the fight against cancer in the future.