Breast Cancer
21.03.2025
BREAST CANCER DIAGNOSIS AND TREATMENT
Breast cancer is a condition in which cells in the breast grow and multiply uncontrollably, forming a tumor. It is one of the most common types of cancer among women worldwide and is rarely seen in men. Early diagnosis is vital; because when detected at an early stage, the chance of treatment increases significantly. Symptoms of breast cancer include changes such as a palpable mass in the breast, change in breast shape, skin shrinkage or discoloration, discharge or indentation of the nipple. Regular breast examination and mammography screenings play a critical role in the early diagnosis of this disease. Raising awareness of breast cancer and the importance of early diagnosis are key factors in treating the disease and increasing survival rates.
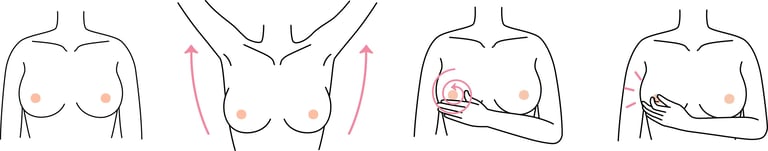
Image 1: It is recommended that every woman after the age of 20 develops awareness about breast cancer and learns to perform breast self-examination.

WHAT ARE THE RISK FACTORS?
Breast cancer risk factors are various factors that affect the likelihood of developing the disease. Among these risk factors, some are modifiable while others are not.
Nonmodifiable Risk Factors
Gender: Breast cancer is much more common in women than in men.
Age: The risk of breast cancer increases with age. Most cases of breast cancer occur in women over the age of 50.
Genetics and Family History: Breast cancer is a complex disease affected by genetic risk factors and familial transmission. The most well-known genetic risk factors are BRCA1 and BRCA2 gene mutations, which have been associated with a high risk of breast and ovarian cancer. Other genetic mutations (such as PALB2, TP53, PTEN, CDH1, and NGO11) may increase the risk of breast cancer. Individuals with a family history of breast cancer have a higher risk, especially when more than one family member is affected or the cancer occurs at an early age. Genetic mutations are usually inherited in an autosomal dominant manner, which means that even a single mutation from just one parent can increase risk. In this context, genetic counseling and testing for individuals with a high family history can help assess risk and determine appropriate screening strategies. The role of genetic factors in breast cancer has an important place in the early diagnosis and management of the disease.
Cancer History: Women who have previously had breast cancer or certain types of breast cell abnormalities (for example, atypical hyperplasia) are at risk of developing cancer again.
Beginning of Menstruation and Menopause: Starting menstruation at an early age (before age 12) or having a late menopause (after age 55) increases the risk.
Dense Breast Tissue: Dense breast tissue can make cancer harder to detect on mammography and may also increase the risk of breast cancer.
Modifiable Risk Factors
Hormone Therapy: Estrogen and progesterone hormone treatments after menopause may increase the risk of breast cancer when used for a long time.
Obesity and Diet: Obesity and high-fat diets in the postmenopausal period may increase the risk.
Lack of Physical Activity: Not exercising regularly (sedentary life) may increase the risk of breast cancer.
Alcohol Consumption: Consuming increased amounts of alcohol increases the risk of breast cancer.
Birth and Breastfeeding History: Having a first birth at a later age or not giving birth at all, as well as not breastfeeding, may also increase the risk.
Exposure to Radiation: Radiation treatments to the chest area at a young age (for example, for Hodgkin lymphoma) may increase the risk.
Although the presence of these risk factors does not mean the development of breast cancer, it is important to understand the existing risks and increase the opportunities for early diagnosis with regular health checks.
Image 2: People with suspected breast cancer should be pre-evaluated by breast surgeons with breast examination, breast ultrasound and mammography.
HOW DOES IT OCCUR?
The mechanisms of breast cancer development involve complex and diverse biological processes. Basically, DNA damage or genetic mutations occur in the cells of the breast tissue, leading to disruption of the normal control mechanisms of the cells. Defects in genes that control the growth and proliferation of cells (oncogenes and tumor suppressor genes) are especially important. For example, BRCA1 and BRCA2 gene mutations play critical roles in repairing cell damage, and their dysfunction can lead to uncontrolled proliferation of cancerous cells. Hormones are also an important factor in the development of breast cancer; Hormones such as estrogen and progesterone can stimulate the growth and proliferation of breast cells. Factors such as environmental factors, lifestyle choices and genetic predisposition also play a role in the development of breast cancer. The combination of these factors causes cells to grow abnormally and ultimately causes breast cancer.
WHAT ARE THE SYMPTOMS?
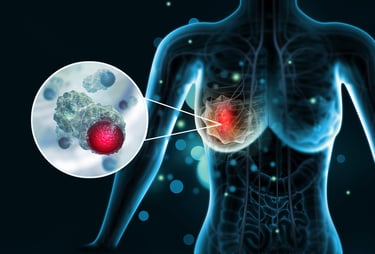
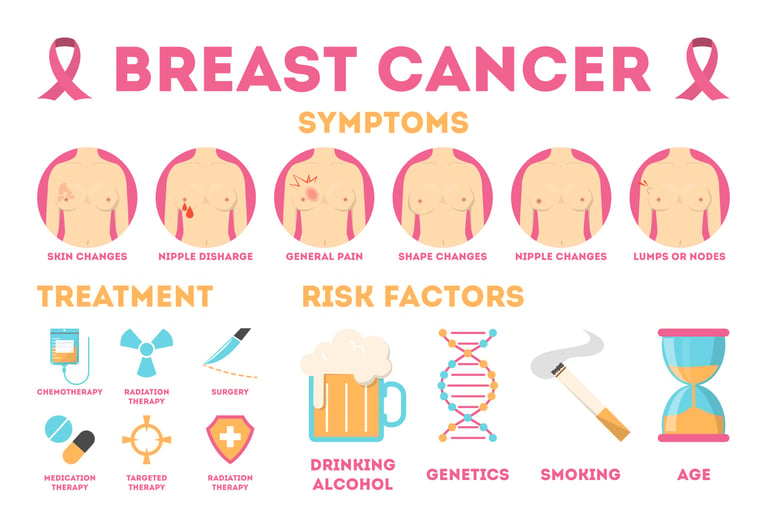
Breast cancer can manifest itself with various symptoms. These symptoms may differ in everyone, but the most common findings are:
Mass or Hardness in the Breast: The most common symptom of breast cancer is a palpable lump or hardness in the breast. This mass is usually painless, but may not always be.
Change in Breast Shape: There may be changes in breast shape or size. These often differ from one breast to the other.
Skin Changes: There may be shrinkage, edema (orange peel appearance), redness or a rough feeling on the breast skin.
Change in Nipple: The nipple may collapse or change shape, and the skin around the nipple may become crusted or flaky.
Discharge from Nipple: There may be abnormal, sometimes bloody, nipple discharge.
Mass or Swelling in the Armpit: Breast cancer sometimes manifests itself with swelling or mass in the lymph nodes under the armpit.
If you notice any of these symptoms, it is important to contact a healthcare provider. Although symptoms do not always mean cancer, they should be evaluated for early diagnosis and intervention.
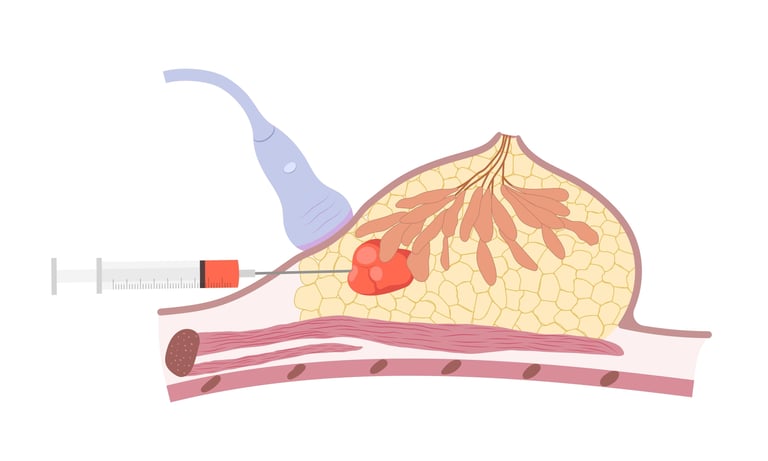
Image 3: People with suspected breast cancer must have a biopsy and pathological examination to clarify the diagnosis.
HOW IS IT DIAGNOSED?
Breast cancer is diagnosed through a comprehensive medical evaluation process. The first step is usually a physical examination of the patient. The doctor looks for signs such as breast lumps, skin changes, or nipple abnormalities. Imaging tests such as mammography are then performed; Mammography plays a key role in detecting abnormal tissue or masses in the breast. If a suspicious mass is found, a biopsy is performed to make a definitive diagnosis; During this procedure, a tissue sample is taken from the mass and examined under a microscope. Tissue samples obtained from biopsy are evaluated pathologically to determine the presence of cancer cells, the type of cancer, and other important characteristics (e.g., hormone receptor status). If necessary, additional imaging tests and genetic tests may be performed to understand the spread of the disease. This multi-stage process ensures an accurate and precise diagnosis of breast cancer.
WHAT ARE THE PATHOLOGICAL TYPES?
Breast cancer is divided into various types and subtypes according to their histopathological characteristics. These pathological types are based on the cellular characteristics of the cancer that appear under the microscope and how it grows in the breast tissue.
Pathological types of breast cancer:
Ductal Carcinoma In Situ (DCIS): It is an early-stage type of breast cancer, and the cancer cells are limited to the milk ducts and have not spread to the surrounding tissues.
Lobüler Carcinoma In Situ (LCIS): LCIS is not considered breast cancer, but it is a condition that increases the risk of developing breast cancer. Cancer cells are limited within the lobules and do not spread to surrounding tissues.
Invasive Ductal Carcinoma (IDC): It is the most common type of breast cancer. This type of cancer starts in the milk ducts and spreads to the surrounding breast tissue.
Invasive Lobular Carcinoma (ILC): This type starts in the mammary lobules (milk-producing glands) and can spread to surrounding tissues. It is the second most common type after IDC.
Medullary Carcinoma: This type is a rare type of invasive carcinoma and usually has a benign course.
Müsinöz (Mukoid) Carcinoma: This is also a rare type and the tumor cells contain mucus.
Tubular Carcinoma: It is a type of carcinoma that forms small, tube-like structures and usually has a good prognosis.
Papillary Carcinoma: This type contains papillary (finger-like) structures and is rarely seen.
Cribriform Carcinoma: It is a rare type of carcinoma that forms porous strainer-like structures.
Metaplastic Carcinoma: This type is a rare and diverse form of breast cancer; The tumor may contain both glandular and non-glandular components.
These pathological types are important in understanding the biological behavior of cancer, its response to treatment, and its prognosis. Pathological evaluation of cancer plays a critical role in determining the appropriate treatment strategy. In addition to pathological types, hormonal receptor status, HER2 status and other molecular features are also taken into account in treatment planning.
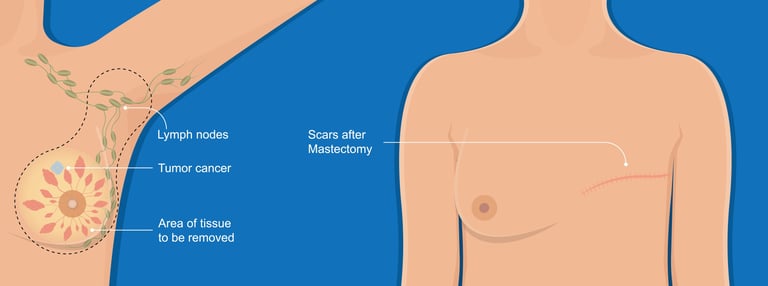
Image 4: The main treatment for early stage breast cancer is surgery. With breast-conserving surgery, there may be no need to completely remove the breast.
WHAT ARE THE PATHOLOGICAL FEATURES?
Breast cancer has several important receptors and proteins that should be considered during pathological evaluation. These receptors determine the biological characteristics of cancer and play a critical role in determining treatment options.
The most important receptors:
Estrogen Receptor (ER): The presence of the estrogen receptor on the surface of breast cancer cells indicates that the growth of cancer is supported by the estrogen hormone. ER-positive cancers may respond to hormone therapy.
Progesterone Receptor (PR): The progesterone receptor similarly indicates that the growth of cancer cells is affected by the hormone progesterone. PR-positive cancers also generally respond well to hormone therapy.
HER2/neu Receptor: HER2 (human epidermal growth factor receptor 2) can be detected in breast cancer cells and may cause the cancer to grow more aggressively. HER2-positive cancers can be treated with targeted therapies (e.g., trastuzumab).
Ki-67: It is a marker of proliferation, which is an indicator of how fast a tumor is growing. High Ki-67 levels may indicate rapidly dividing cells and more aggressive cancer.
The presence and levels of these receptors and proteins are determined using immunohistochemical staining and other laboratory tests. This information provides important clues about how to treat cancer. For example, while hormone therapy may be effective in ER and PR positive cancers, targeted therapies are preferred in HER2 positive cancers. Therefore, pathological evaluations of patients diagnosed with breast cancer play a fundamental role in treatment planning.
HOW IS STAGING DONE IN BREAST CANCER?
Staging in breast cancer is a system used to determine how far the cancer has spread in the body. Staging is critical for treatment planning and prognosis prediction.
Tumor Size (T): Staging evaluates the size of the tumor or how far the cancer cells have spread in the breast. Tumors are classified from microscopic (very small, undetectable by imaging tests) to large tumors.
Spread to Lymph Nodes (N): Spread to lymph nodes determines whether cancer cells have reached nearby lymph nodes. The presence of cancer cells in regional lymph nodes increases the risk of the disease spreading to other parts of the body.
Distant Metastases (M): It is examined to see if the cancer has spread to other parts of the body (for example, bones, lungs, liver, or brain). Distant metastases indicate that the disease is at a more advanced stage.
These three components (T, N, M) are known as the TNM classification system and are evaluated together to determine the stage of the cancer. Breast cancer is generally classified into stages 0 through IV:
Stage 0: It represents cancer in situ, meaning the cancer cells are confined to the original tissue and have not spread to surrounding tissues.
Evre I - II: Early stage breast cancer; The tumor is usually small and may have spread to a limited number of lymph nodes.
Stage III: Advanced local breast cancer; There are larger tumors or extensive lymph node involvement.
Stage IV: Metastatic breast cancer; The cancer has spread to other parts of the body.
Staging may also include the hormone receptor status of the tumor and HER2/neu gene expression. These factors are important in determining treatment options and predicting prognosis. Staging; It is done based on medical imaging, biopsy and physical examination findings.
Image 5: Treatment success in breast cancer; It is extremely important to reduce risk factors, perform regular screening and start treatment with early diagnosis.
HOW IS BREAST CANCER TREATMENT ACCORDING TO STAGES?
Breast cancer treatment varies depending on the stage of the cancer and often involves more than one treatment method. Here are general treatment approaches according to different stages of breast cancer:
Stage 0 (In Situ Cancer)
Surgery: Lumpectomy (removal of cancerous tissue and some surrounding healthy tissue) or mastectomy (removal of all breast tissue).
Radiotherapy: Sometimes performed after lumpectomy to prevent cancer cells from reoccurring in the area.
Hormone Therapy: It can be used to reduce the risk of cancer returning in hormone receptor-positive cancers.
Early Stage Breast Cancer (Stage I and II)
Surgery: Lumpectomy or mastectomy may be performed. Lymph nodes may also be intervened (sentinel lymph node biopsy or axillary lymph node dissection).
Radiotherapy: May be performed if lumpectomy was performed after surgery to prevent regional recurrence of cancer.
Chemotherapy: In cases with high risk of spread, it can be applied before (neoadjuvant) or after (adjuvant) surgery.
Hormone Therapy and Targeted Therapies: It is preferred in hormone receptor positive or HER2 positive cancers.
Locally Advanced Breast Cancer (Stage III)
Neoadjuvant Therapy: Chemotherapy or targeted therapies may be used to shrink the tumor before surgery.
Surgery: Mastectomy or lumpectomy may be performed. Extensive lymph node dissection may be performed.
Radiotherapy: It can be performed after surgery, especially if the lymph nodes are affected.
Adjuvant Therapy: Chemotherapy, hormone therapy, or targeted therapies may be administered after surgery to reduce the risk of cancer returning.
Metastatic Breast Cancer (Stage IV)
Systemic Therapies: Treatments such as chemotherapy, hormone therapy, targeted therapies, and immunotherapy are used to keep cancer under control and relieve symptoms.
Palliative Care: Supportive treatments can be applied to improve the patient's quality of life and relieve symptoms.
Local Treatments: In some cases, surgery or radiotherapy may be used to control cancer in certain areas or reduce symptoms.
The treatment plan for each patient is personalized based on factors such as the biological characteristics of the cancer, general health status, personal preferences, and response to treatment. Treatment is managed by oncologists, surgeons, radiation oncologists and other healthcare professionals with a multidisciplinary approach.
SYSTEMIC DRUG GROUPS USED IN TREATMENT
Drugs used to treat breast cancer are wide-ranging and include chemotherapies, hormonal treatments, targeted (smart) drugs, and immunotherapies. Each type of treatment is customized based on the characteristics of the cancer and the needs of the patient.
Some examples of these treatments:
Chemotherapy drugs
Chemotherapy is used to prevent the growth and spread of cancer cells.
Common used chemotherapies:
Anthracyclines (e.g. Doxorubicin, Epirubicin)
Taxanes (e.g. Paclitaxel, Docetaxel)
Alkylating Agents (e.g. Cyclophosphamide)
Fluoropyrimidines (e.g. 5-Fluorouracil)
Platinum-Based Agents (e.g. cisplatin, carboplatin)
Hormonal Treatments
It is used in hormone receptor positive breast cancers. These treatments block or reduce the effects of estrogen on cancer cells:
Tamoxifen
Aromatase Inhibitors (e.g. Anastrozole, Letrozole, Exemestane)
Selective Estrogen Receptor Downregulators (SERDs), örn. Fulvestrant
Targeted (Smart) Drugs
These drugs are designed to target specific molecular targets in cancer cells:
Trastuzumab is used in HER2 positive breast cancers.
Pertuzumab is often used together with Trastuzumab for HER2-positive cancers.
Lapatinib is used in HER2-positive cancers.
CDK4/6 Inhibitors (e.g. Palbociclib, Ribociclib, Abemaciclib) are used in hormone receptor-positive, HER2-negative advanced breast cancer.
PI3K Inhibitors (e.g. Alpelisib) are used in hormone receptor positive, HER2 negative advanced breast cancers with PIK3CA mutation.
Immunotherapies
Immunotherapy aims to strengthen the immune system to fight cancer: Pembrolizumab and Atezolizumab are used in certain conditions, especially PD-L1 positive breast cancer.
The selection and combination of these treatments are customized by doctors depending on the biological characteristics of the cancer, the patient's general health status, response to treatment, and side effects of treatment. Supportive care also plays an important role during the treatment process to manage the patient's quality of life and treatment side effects.
WHAT IS THE LIFE EXPECTANCY WITH BREAST CANCER?
The life expectancy of people diagnosed with breast cancer can vary depending on many factors and has improved significantly in recent years thanks to developments in this field. Key factors affecting life expectancy include the stage of the cancer, biological characteristics of the tumor (e.g. hormone receptor status and HER2 status), general health status, response to treatment, and early diagnosis. Breast cancers detected at an early stage generally have a better prognosis; because at this stage the cancer is more sensitive to treatment, has not spread, and treatment options are wider. Advanced breast cancers require more complex treatment approaches and the prognosis is generally more difficult. However, thanks to the advanced treatment methods and individualized treatment plans offered by modern medicine, many patients can live a longer and higher quality life. Additionally, constantly evolving medical research and new treatment strategies offer promising advances in the fight against breast cancer. In summary, life expectancy with breast cancer is unique to the individual and is constantly improving thanks to various treatment approaches and ever-improving medical care.
HOW SHOULD THE FOLLOW-UP BE DONE AFTER RECOVERY OF BREAST CANCER?
Follow-up after recovery from breast cancer is vital to detect early recurrence of the disease and ensure long-term health management. This follow-up process usually includes regular physical exams, breast exams, and mammograms. Doctors usually recommend a physical exam every 3-6 months and annual mammograms for the first few years. Patients are also encouraged to perform breast self-exams and contact their doctor immediately if they notice any changes, lumps, pain, or other abnormalities. In hormone receptor-positive cancers, hormone therapy is usually continued for 5 to 10 years. Additionally, supportive health strategies such as lifestyle changes, a balanced diet, and regular exercise also help improve patients' overall well-being. During this process, patients receiving emotional and psychological support is also an important part of the recovery process. In general, follow-up after recovery from breast cancer requires a multidisciplinary approach and is conducted through constant communication between the patient, oncologist, radiologist, and other healthcare professionals.
WHAT ARE THE SCREENING TESTS FOR FAMILY MEMBERS?
Early diagnosis of breast cancer is critical for successful treatment of the disease, and various screening tests are at the center of this process. The most common and effective screening method is mammography; It enables the detection of abnormal tissues and masses in the breast using low-dose X-rays. Mammography is especially recommended for women age 40 and over and is usually performed every year or two. For individuals at high risk, earlier and more frequent mammography screenings are generally recommended. Ultrasound can be used in addition to mammography, especially for women with dense breast tissue, which helps detect smaller lesions. In some cases, especially in high-risk individuals, breast magnetic resonance imaging (MRI) may be recommended. MRI can show lesions that mammography and ultrasound cannot detect. Genetic counseling and genetic testing such as BRCA1/BRCA2 may also be recommended for individuals who are at high risk due to family history or genetic factors. When these screening tests are performed regularly, they allow breast cancer to be detected in the early stages and more effective treatment options to be used.