Testicular Cancer
21.03.2024
TESTICULAR CANCER DIAGNOSIS AND TREATMENT


Testicular cancer is a type of cancer characterized by abnormal and uncontrolled growth of cells in the testicles. An essential part of the male reproductive system, the testicles produce sperm and male sex hormones. Testicular cancer usually occurs in young and middle-aged men, and its most common symptoms include a swelling or lump in the testicle, pain or discomfort. When diagnosed early, testicular cancer is often very highly treatable, highlighting the importance of early diagnosis. Treatment methods include surgery, chemotherapy and radiation therapy. Since testicular cancer is one of the most common types of cancer, especially among young men, it is important to raise awareness of this type of cancer and for men to examine themselves regularly. Recognizing early symptoms and seeking medical help quickly can significantly increase treatment success and improve long-term health outcomes.
WHAT ARE THE RISK FACTORS?
There are some known risk factors for testicular cancer, but not all of these factors mean you will get cancer. The main known risk factors of testicular cancer are:
Family History: The risk may increase in people with a family history of testicular cancer.
Personal History: People who have previously had cancer in one testicle have a higher risk of developing cancer in the other testicle.
Age: Testicular cancer usually occurs in young men between the ages of 15 and 35, but it can occur at any age.
Race and Ethnicity: It is more common in white men living in North America, Europe and Australia than in men of African or Asian descent.
Abnormal Testicular Development: Abnormalities in the normal development of the testicles, such as cryptorchidism (undescended testicles), may increase the risk of testicular cancer.
HIV Infection/AIDS: The risk of testicular cancer is slightly higher in men who are HIV positive.
Body Size: Some studies have shown that taller men have a slightly higher risk of testicular cancer.
Congenital Abnormalities: Congenital abnormalities such as undescended testicles, hydrocele (accumulation of fluid in the scrotum), or abnormal development of the testicles may increase the risk.
Environmental and Lifestyle Factors: Some studies show that exposure to certain chemicals or certain lifestyle choices may affect testicular cancer risk, but these relationships are not clear.
These factors do not mean that any man will develop testicular cancer, but those with these risk factors are advised to have regular health checks and report any abnormal findings to their doctor. Early diagnosis plays a very important role in the successful treatment of testicular cancer.
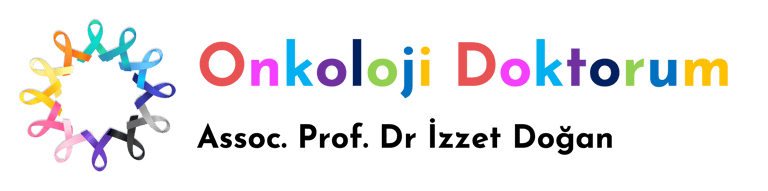
Image 1: In testicular cancer, testicular swelling, pain, and breast enlargement (gynecomastia) due to hormone release may occur.
HOW DOES IT OCCUR?
Testicular cancer begins when cells in the testicles divide and multiply in an uncontrolled and abnormal manner, but the exact mechanism of this process is not fully understood. Genetic mutations can trigger this cell growth, disrupting the normal growth and death cycles of cells and leading to the accumulation of abnormal cells. The specific genetic and molecular pathways involved in the development of testicular cancer are still being actively investigated. In some cases, abnormalities in the normal development of the testicles in early life (for example, undescended testicles) may increase the risk of cancer. Additionally, some environmental factors and lifestyle choices may also affect risk. Genetic predisposition is also an important factor; People with a family history of testicular cancer are especially at higher risk. There is an interaction of more than one factor in the development of testicular cancer, and the details of these interactions are still a matter of research. Therefore, scientific studies on testicular cancer continue to contribute to a better understanding of the disease and the development of effective treatment methods.
WHAT ARE THE SYMPTOMS?
Signs and symptoms of testicular cancer are diverse, and detection at an early stage is very important for the success of treatment.
Common symptoms of testicular cancer:
Softness or Swelling in the Testicles: It is usually the most common symptom of cancer. A painless lump or swelling is usually felt in the testicle.
Change in Testicular Size or Shape: An abnormal change in the growth or shape of the testicle may be detected.
Pain or Discomfort: There may be pain or discomfort in the testicle, groin, lower abdomen or scrotum.
Painful or Painless Testicular Enlargement: One of the testicles may become larger than the other.
Feeling of Heaviness: There may be a feeling of heaviness or fullness in the scrotum.
Fluid Accumulation: A sudden accumulation of fluid may occur in the scrotum.
Changes in Breast Tissue: Rarely, testicular cancer can affect hormone balance and lead to changes in breast tissue, such as enlargement or tenderness.
Backache: In advanced stage testicular cancer, lower back pain may occur due to the spread of the cancer.
It is important for men to see a doctor for a medical evaluation if they experience any of these symptoms. Early diagnosis plays a vital role in successfully treating testicular cancer. Not all of these symptoms necessarily indicate testicular cancer, but they need to be evaluated by a physician.
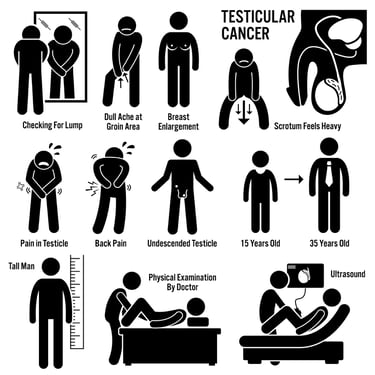
HOW IS IT DIAGNOSED?
Diagnosis of testicular cancer usually goes through a several-stage process. The first step is finding an abnormal lump or swelling in the testicle, usually noticed by the patient himself or discovered during a doctor's physical examination. The doctor detects abnormalities by performing a physical examination of the testicles and scrotum. If cancer is suspected, imaging tests such as ultrasonography are used. Ultrasound allows a more detailed examination of the abnormal tissue in the testicle. A blood test is usually performed to confirm the diagnosis, looking for levels of testicular cancer markers alpha-fetoprotein (AFP), beta human chorionic gonadotropin (β-hCG) and lactate dehydrogenase (LDH). If these tests and examination findings raise the possibility of cancer, a tissue sample from the testicle or surgical removal of the entire testicle may often be necessary to confirm the diagnosis. This surgical procedure is known as orchiectomy, and the tissue sample is sent for pathological examination. Pathology results help determine the type and extent of cancer. These tests and evaluations allow doctors to determine the presence and stage of testicular cancer and plan appropriate treatment options. Early diagnosis plays an important role in the treatment of testicular cancer and greatly affects patient survival and treatment success.
WHAT ARE THE PATHOLOGICAL TYPES?
Testicular cancer is divided into different types according to their pathological characteristics. These types are classified based on how cancer cells look under a microscope and the type of cell from which the cancer originates. Here are the most common pathological types of testicular cancer:
Seminomas: Seminomas, which make up approximately half of testicular cancers, are generally slower growing and respond better to treatment.
Nonseminomatous Germ Cell Tumors: These types tend to grow more aggressively and usually appear at a younger age than seminomas. Nonseminomatous tumors include the following subtypes:
Embryonic Carcinoma: It is a highly malignant and aggressive species.
Yolk Sac Tumor (Endodermal Sinus Tumor): It is more common in children.
Choriocarcinoma: It is a very rare, but extremely aggressive type.
Teratoma: It is a type with variable behavior that can contain different tissue types.
Mixed Germ Cell Tumors: These types include more than one type of germ cell tumor and can display a variety of pathological features.
Stromal Tumors: They are rare tumors arising from testicular stromal cells, such as Leydig cell tumors and Sertoli cell tumors.
The pathological type of testicular cancer plays an important role in determining treatment options and prognosis. While seminomas are generally more sensitive to radiation, nonseminomatous germ cell tumors usually require more aggressive treatment. Therefore, accurate pathological diagnosis is critical for determining appropriate treatment strategies. Each species differs in its biological behavior and response to treatment, which is an important factor to consider in treatment planning. In the diagnosis and treatment of testicular cancer, it is especially important to look at some biological markers and molecular receptors. These markers play a critical role in determining the type of cancer, its stage, and its response to treatment. The most commonly used markers include Alpha-Fetoprotein (AFP) and Beta-Human Chorionic Gonadotropin (β-hCG). While AFP is usually elevated in nonseminomatous germ cell tumors, β-hCG may be elevated in both seminoma and nonseminomatous tumors. Additionally, general tumor markers such as Lactate Dehydrogenase (LDH) are also used to evaluate tumor burden and response to treatment. In some cases, markers such as Ki-67, which indicate cellular proliferation of the tumor, can also be evaluated. Levels of these markers are vital in diagnosing testicular cancer, planning treatment, and monitoring the course of the disease. These markers need to be checked regularly to evaluate response to treatment and monitor the potential for disease relapse. This approach allows the disease to be detected at an early stage and a more effective treatment plan to be created.
Image 2: Examination and testicular ultrasound can be used to diagnose testicular cancer.
HOW IS TUMOR STAGING DONE?
Tumor staging in testicular cancer is a process used to determine how far the cancer has spread and is important in evaluating treatment options and prognosis. It is usually performed according to the TNM (Tumor, Node, Metastasis) system:
T - Tumor Size and Local Spread:
T1: The tumor is limited to the testicle.
T2: The tumor has spread beyond the testicle but has not penetrated the spermatic cord or scrotum wall.
T3: The tumor has spread to the spermatic cord.
T4: The tumor has spread to the scrotum wall.
N - Regional Lymph Nodes:
N0: There is no metastasis in regional lymph nodes.
N1-3: Varies depending on the size and number of metastases in the lymph nodes.
M - Distant Metastasis:
M0: There is no distant metastasis.
M1: There is distant metastasis, divided into M1a and M1b substages (M1a usually refers to lung metastasis, M1b refers to other organ metastases).
Serum Tumor Markers:
In testicular cancer, serum tumor markers (AFP, β-hCG, LDH) are also included in staging. The levels of the markers provide information about the aggressiveness of the disease and its response to treatment.
TNM classification evaluates the local spread of the tumor and its metastasis to regional lymph nodes and distant organs. Additionally, other diagnostic methods such as imaging tests (CT, MRI, PET scans) and biopsy also help with staging. Staging is used to determine treatment options (surgery, chemotherapy, radiation therapy) and predict the patient's overall prognosis. Early-stage testicular cancer generally has high treatment success, so an accurate and detailed staging process is important.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Testicular cancer treatment is determined by the stage of the disease and requires a specific approach for each patient.
General treatment methods according to different stages of testicular cancer:
Stage I (Cancer Only in Testis)
Radical Orchiectomy: Surgical removal of the affected testicle. This forms the basis of treatment for testicular cancer in all stages.
Active Monitoring: Unless there are signs of cancer recurrence after surgery, no additional treatment is given, but regular monitoring is required.
Radiation Therapy: Can be used in some types of seminoma.
Chemotherapy: It may be preferred for nonseminomatous tumors with a high risk of recurrence.
Stage II (Spread to Regional Lymph Nodes)
Radical Orchiectomy and Chemotherapy: It is the main treatment method for seminoma and nonseminoma.
Radiation Therapy: May be preferred for seminomas, especially in cases with small tumor burden in the lymph nodes.
Stage III (Distant Metastasis)
Chemotherapy: It is the main treatment option for advanced testicular cancer. Various drug combinations are used.
Surgery: In some cases, remaining disease after chemotherapy may need to be surgically removed.
Radiation Therapy: May be used in some cases of seminoma or to treat certain metastatic lesions.
Treatment varies depending on the type of disease and the patient's general health condition. Seminoma and nonseminoma testicular cancers may respond to different treatment approaches. Testicular cancer is a type of cancer with high recovery rates with early diagnosis and appropriate treatment. During the treatment process, the patient is supported with regular follow-up and additional treatment options when necessary. The prognosis for early-stage testicular cancer is usually excellent, and even in advanced-stage disease, the chance of recovery is high.
Image 3: Testicular cancer treatment is planned by urology, medical oncology and radiation oncology physicians as a multidisciplinary team.
WHAT ARE THE DRUGS USED IN TREATMENT?
There are various drugs and treatment methods used in the treatment of testicular cancer. These treatments vary depending on the type and stage of cancer. Here are the main types of treatments and drugs used in testicular cancer:
Chemotherapy
BEP (Bleomycin, Etoposide, Cisplatin): It is the most commonly used chemotherapy regimen.
EP (Etoposide, Cisplatin): Used in case of intolerance to Bleomycin.
VIP (Vinblastine, Ifosfamide, Cisplatin): It is an alternative option for cases that do not respond to other regimens.
TIP (Paclitaxel, Ifosfamide, Cisplatin): Used for cases resistant to other treatments.
Smart Drug Therapies (Targeted Therapies)
Specific targeted ("smart") therapies are not widely used in the treatment of testicular cancer. However, research is ongoing in this area.
Immunotherapies
Pembrolizumab: It is being investigated in some cases of advanced or treatment-resistant testicular cancer.
Combination of Nivolumab and Ipilimumab: Being tested in some clinical trials.
The basic approach to testicular cancer treatment is usually surgery and chemotherapy. However, depending on the type of cancer and the individual condition of the patient, various treatment options may be considered in addition to these treatments. The treatment process is individualized, taking into account factors such as the patient's general health condition, the characteristics of the cancer and the response to treatment. The treatment plan is reviewed regularly and adjustments are made if necessary.
HOW SHOULD FOLLOW-UP BE DONE AFTER RECOVERY?
Follow-up after recovery from testicular cancer is critical to detect early disease recurrence and monitor long-term health status. This process usually begins after surgery or chemotherapy treatment and can take several years. The follow-up program includes regular physical examinations, blood tests (especially checking levels of tumor markers alpha-fetoprotein (AFP) and beta human chorionic gonadotropin (β-hCG)), and periodic imaging tests (for example, computed tomography (CT) scans). During the first few years, these checks are usually done more frequently because the risk of recurrence is higher during this period. Over time, the frequency of follow-up may be reduced for patients who show no symptoms. In addition, long-term side effects of testicular cancer treatment, especially cardiovascular disease and the risk of a second cancer, should be monitored with regular health checks. The patient should contact their healthcare provider immediately with any new symptoms or concerns. A comprehensive follow-up program helps maintain the patient's overall health and maximize quality of life.