Sarcomas
21.03.2025
SOFT TISSUE TUMOR (SARCOMA) DIAGNOSIS AND TREATMENT
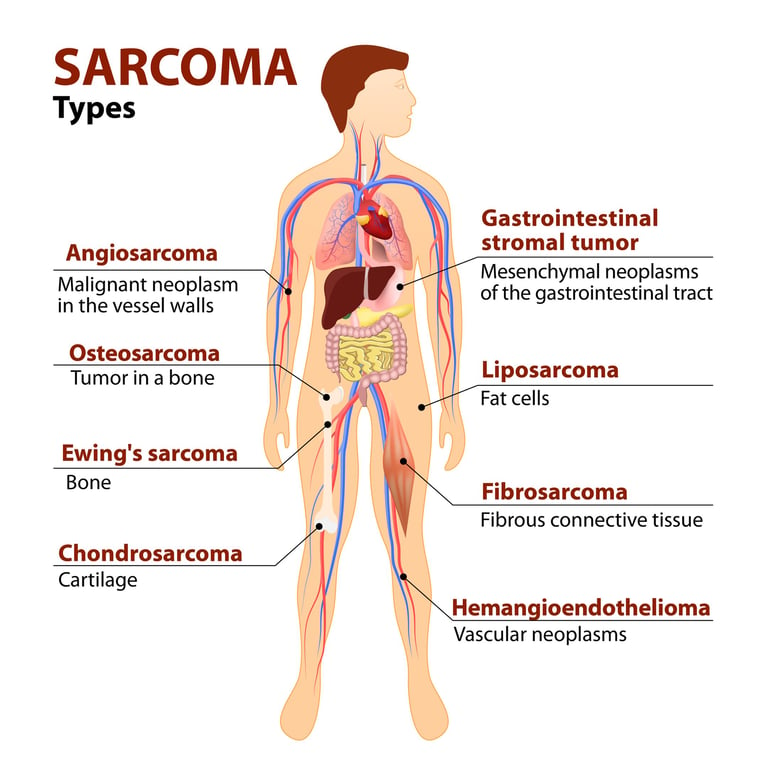
Sarcoma is a type of cancer that originates from the body's connective tissue cells (such as bone, muscle, fat, nerve tissue and blood vessels). Sarcomas can occur almost anywhere in the body, but occur most frequently in the legs, arms, and trunk. Sarcomas are divided into two main groups: bone sarcomas and soft tissue sarcomas. Treatment options include surgery, radiotherapy and chemotherapy, and early diagnosis is vital. Although sarcomas are rarer than other types of cancer, they can affect people of all ages. The severity of the disease and response to treatment may vary depending on the type of sarcoma, its size, location, and the patient's general health condition. Therefore, increasing awareness of sarcoma and promoting early diagnosis is critical to increasing patients' survival rates.
WHAT ARE THE RISK FACTORS?
There are various factors that can increase the risk of developing sarcoma, but the exact cause of this type of cancer is often unknown. Some risk factors that may play a role in the development of sarcoma include:
Genetic Conditions: Some genetic diseases may increase the risk of developing sarcoma. For example, genetic disorders such as Li-Fraumeni syndrome, neurofibromatosis, Gardner syndrome, and retinoblastoma may increase the risk of sarcoma.
Exposure to Radiation: Especially in people who received radiation therapy in childhood, the risk of developing sarcoma may increase in the following years. Additionally, exposure to high doses of radiation (for example, during nuclear reactor accidents) may also increase the risk.
Chemical Exposures: Exposure to certain chemicals, especially some herbicides and arsenic, may increase the risk of sarcoma.
Chronic Inflammation: Long-term inflammation or chronic wounds may increase the risk of developing certain soft tissue sarcomas.
With Viral Infection: Some viruses, such as human immunodeficiency virus (HIV) or Epstein-Barr virus, may increase the risk of sarcoma.
Age and Gender: Some types of sarcoma are more common in certain age groups or genders, but this type of cancer can affect people of all ages.
Cancer Treatment History: In particular, some cancer treatments (such as chemotherapy and radiotherapy) may increase the risk of sarcoma in the past.
Each of these factors can increase the risk of developing sarcoma, but most cases of sarcoma have no specific cause. Additionally, the presence of these risk factors does not mean that sarcoma will develop; It just shows that the risk is slightly higher. Maintaining a healthy lifestyle and regular medical check-ups can help minimize risks.
Image 1: Sarcomas are cancers that develop in soft tissues such as muscle, fat and vessels in the body.


HOW DOES IT OCCUR?
The mechanisms of development of sarcoma are associated with a complex interaction of genetic and environmental factors. Sarcomas are characterized by abnormal and uncontrolled cell growth in the cells that make up the body's connective tissue (such as bone, muscle, fat, nerve tissue, blood vessels). This abnormal growth usually begins as a result of mutations in the cells' DNA. These mutations lead to dysfunction of genes that regulate cell division and death. Normally, these genes ensure that cells grow properly, divide, and die on time; However, mutations cause this balance to be disrupted and cells to proliferate uncontrollably. Additionally, some genetic syndromes and environmental factors (such as radiation, chemical exposure) may contribute to the formation of these mutations. Sarcoma cells spread to surrounding tissues over time and metastasize to distant organs, causing the disease to progress. Each type of sarcoma is characterized by different genetic alterations and environmental interactions, leading to significant variation in diagnosis and treatment processes.
WHAT ARE THE SYMPTOMS?
Symptoms of sarcoma may vary depending on the type of cancer and its location. However, some common findings include:
Mass or Swelling: The most common symptom is a noticeable mass or swelling in the affected area. This mass is usually painless.
Pain: As the mass grows, it can put pressure on the nerves or surrounding tissues and cause pain. If the sarcoma is in the bones, the pain is usually more pronounced.
Loss of Function or Limitation of Movement: If sarcoma is in muscles or near joints, it may cause limitation of movement or loss of function.
Bone Fractures: Bone sarcomas can cause the affected bones to weaken, which can lead to unexpected or easy fractures.
Fatigue and Weakness: Many types of cancer, including sarcoma, can cause general feelings of tiredness and weakness.
Weight Loss: Unexplained weight loss can be a symptom of various types of cancer, including sarcoma.
Fever and Sweating: Fever and sweating, especially at night, may be seen in some sarcoma patients.
If you have any one or more of these symptoms, especially if they persist for a long time or worsen, it is important to see a healthcare professional for medical evaluation and diagnosis. Early diagnosis of sarcoma can significantly increase treatment success.
HOW IS IT DIAGNOSED?
Sarcoma is usually diagnosed through a combination of multiple medical tests and procedures. The first step usually begins with the patient's complaints and physical examination. The doctor evaluates the symptoms and checks the body for abnormal masses or swellings. If there is a suspicious mass, imaging tests are performed; these include ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), and sometimes positron emission tomography (PET). These imaging methods are used to evaluate the size, location, and impact of masses on surrounding tissues. Definitive diagnosis is usually made by biopsy; In this procedure, a small sample of suspicious tissue is taken and examined under a microscope. The pathologist examines this tissue sample to determine the presence of cancerous cells and the type of cancer. If necessary, genetic tests and other laboratory studies may also be performed. This comprehensive evaluation process is critical to determine the type of sarcoma, its stage, and the most appropriate treatment methods.
WHAT ARE THE PATHOLOGICAL TYPES?
Sarcoma can be divided into a wide variety of histological subtypes, which are generally grouped into two main categories: bone sarcomas and soft tissue sarcomas. Each type arises from different cell types and has unique properties.
Some common types of sarcoma:
Soft Tissue Sarcomas
Liposarcoma: It originates from fatty tissue and is usually seen in adults.
Leiomyosarkom: It develops from smooth muscle cells and is often found in the uterus, stomach and intestines.
Rhabdomyosarcoma: It originates from skeletal muscle cells and occurs most often in children and young adults.
Synovial Sarcoma: It usually occurs near joints, especially in the arms and legs.
Fibrosarcoma: It originates from connective tissue and is usually found in soft tissues outside of bones.
Angiosarcoma: It originates from blood and lymph vessels and affects vascular structures.
Bone Sarcomas
Osteosarcoma: It is the most common type of bone cancer, usually occurs in long bones (legs, arms) and often occurs in young people.
Chondrosarcoma: It develops from cartilage cells and is usually found in the pelvis, thighs and shoulders.
Ewing Sarcoma: It is usually found in bones or soft tissues near bones and is more common in children and young adults.
Each type of sarcoma is characterized by specific molecular and genetic features and plays an important role in determining diagnosis and treatment options. Each of these types differs in how the disease progresses and how it is treated. Therefore, patients diagnosed with sarcoma need customized treatment plans tailored to the specific type and stage of their disease.
In the treatment of sarcoma, it is important to examine various receptors and molecular markers to accurately characterize the disease and create an effective treatment plan. This examination is usually performed during pathological analysis of biopsy samples. Particularly in soft tissue sarcomas, genetic mutations or amplifications such as hormone receptors (e.g., estrogen and progesterone receptors), HER2/neu receptor, and MDM2 and CDK4 in some sarcoma subtypes are examined. Additionally, in some types of sarcoma, PD-L1 expression and other immunohistochemical markers are used to evaluate the effectiveness of immunotherapy. Genetic testing is also done to detect specific genetic translocations and mutations; this is particularly important in types such as Ewing sarcoma and alveolar soft tissue sarcoma. The goal of this molecular profiling is to better understand the disease, determine the most appropriate treatment strategies for patients, and potentially use targeted therapies. Molecular characterization of sarcoma is becoming increasingly important as part of personalized cancer therapy. This approach may help improve patients' prognosis and optimize treatment responses.
Image 2: Sarcoma is diagnosed through imaging tests and biopsy.
HOW IS TUMOR STAGING DONE?
Tumor staging in sarcoma is a process used to determine the extent and severity of the disease. This process evaluates tumor size, local spread, spread to lymph nodes, and metastasis (spread of tumor to other parts of the body). Sarcoma staging usually takes the following steps:
Tumor Size and Location (T): Staging determines how large the tumor is and where it is located. This information is usually obtained through imaging tests such as an MRI, CT or PET scan.
Spread to Lymph Nodes (N): It is examined whether the sarcoma has spread to the lymph nodes. Spread to lymph nodes is more common in some types of sarcoma.
Metastasis (M): Various tests are used to determine whether the tumor has spread to other parts of the body, especially the lungs, liver, or other bones.
Histological Grade: Microscopic examination of the tumor determines how abnormal the cells are and how quickly they are dividing. Higher grade (more aggressive) tumors generally have a worse prognosis.
TNM System: Based on Tumor (T), Lymph Nodes (N) and Metastasis (M) status, the tumor is staged using the TNM classification system. This system divides the stage of the tumor into a series of categories, from I to IV, where I represents the least disseminated and IV represents the most disseminated.
AJCC Staging System: This system, developed by the American Joint Committee on Cancer (AJCC), classifies sarcoma from stages I to IV, taking into account TNM values, the histological grade of the tumor, and sometimes the location of the tumor.
This staging process is vital in sarcoma treatment planning and prognosis assessment. Stage I generally offers a better prognosis, while stage IV indicates cancer that is more advanced and often more difficult to treat. Staging also plays an important role in decisions about participation in clinical trials and other decisions regarding patient care.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Treatment of sarcoma is determined by the stage, type and location of the disease, the patient's general health condition and other factors. General treatment approaches for the different stages of sarcoma include:
Stage I (Early Stage)
Surgical: The main method of treating early stage sarcomas is surgery. Its purpose is to remove the tumor and some of the surrounding healthy tissue.
Radiotherapy: In some cases, radiotherapy may be used in addition to surgery or if surgery is not possible.
Chemotherapy: In some high-grade tumors, chemotherapy may be administered before or after surgery.
Stage II and Stage III (Locally Advanced Stages)
Surgery: Tumors in these stages are usually larger or have more aggressive features. Surgery is used to remove the entire tumor.
Radiotherapy and chemotherapy: In these stages, radiotherapy and/or chemotherapy are often applied in addition to surgery. These treatments can be given before (neoadjuvant) or after (adjuvant) surgery.
Stage IV (Metastatic Sarcoma)
Metastasis Treatment: In the treatment of metastatic sarcoma, special treatments can be applied to the organs where the cancer has spread.
Systemic Treatment: Systemic treatments such as chemotherapy, targeted therapies, and immunotherapy are used to control the spread of cancer to other parts of the body.
Supportive Care: Additionally, supportive care treatments are also important to improve patients' quality of life and relieve symptoms.
At each stage, the treatment plan is personalized and adjusted to the patient's specific condition, type of sarcoma, and other health factors. Innovative treatment approaches and clinical studies may offer new treatment options, especially for advanced sarcomas. Patients' treatment plans should be evaluated by a multidisciplinary team and the treatment options that best suit the patient's needs should be determined.
Image 3: Surgery, radiotherapy, chemotherapy and smart drugs can be used during sarcoma treatment.

WHAT ARE THE SYSTEMIC DRUGS USED IN TREATMENT?
The medications and treatment methods used in the treatment of sarcoma may vary depending on the type of sarcoma, its stage and the general health condition of the patient.
Some common treatments and medications used in sarcoma:
Chemotherapy Drugs
Doxorubicin (Adriamycin)
İfosfamide
Etoposide
Cisplatin and Carboplatin
Vinkristin
Cyclophosphamide
Dactinomycin
Gemcitabine
Smart Drug Therapies (Targeted Therapies)
Imatinib: It is especially used for gastrointestinal stromal tumors (GIST).
Sunitinib
Pazopanib
Trabectedin: Used especially for liposarcoma and leiomyosarcoma.
Olaratumab: Used when combined with doxorubicin.
Immunotherapies
Nivolumab
Pembrolizumab
Ipilimumab: Often used together with nivolumab.
Each of these medications may be appropriate for certain types and characteristics of sarcoma. Additionally, the side effects, effectiveness, and suitability of these treatments for the patient's particular condition must be carefully evaluated. Treatment choices are usually determined after a comprehensive evaluation by oncologists, and personalized treatment approaches are becoming increasingly important in modern cancer treatment. A multidisciplinary approach and a specific assessment of the patient's condition are required to make decisions about the use and combinations of these drugs.
HOW SHOULD FOLLOW-UP BE DONE AFTER RECOVERY?
After completion of sarcoma treatment, regular follow-up is important to reduce the patient's risk of recurrence or metastasis and to monitor their general health status. Post-recovery follow-up is often customized based on the type of sarcoma the patient was initially diagnosed with and their response to treatment. This follow-up is usually done more frequently during the first few years because the risk of recurrence is higher during this period. The follow-up process includes regular physical examinations, laboratory tests, and imaging tests (such as MRI, CT) when necessary. These tests are done to check whether the cancer has returned or spread to another area. Additionally, supportive care and rehabilitation to improve patients' quality of life and manage long-term side effects of treatment are also important. Services such as psychological support, physical therapy, and nutritional counseling can be part of the recovery process. Patients should contact their doctor immediately with any new symptoms or concerns. This comprehensive monitoring and support helps optimize patients' both physical and emotional recovery and enables early detection of relapse or other health problems.