Prostate Cancer
21.03.2025
PROSTATE CANCER DIAGNOSIS AND TREATMENT


Prostate cancer is a type of cancer that begins in the prostate gland cells in men. The prostate gland is part of the male reproductive system, located just below the bladder and produces some of the seminal fluid. Prostate cancer usually develops slowly and may initially remain within the boundaries of the prostate gland, in which case it may not cause serious health problems. However, in some cases, it can grow more aggressively and spread (metastasize) to other parts of the body. Early diagnosis is an important factor in prostate cancer treatment. Various risk factors such as age, genetic factors and lifestyle may play a role in the development of this type of cancer. While it usually does not cause any symptoms in the early stages, it may show symptoms such as urination difficulties, pelvic pain and sometimes bloody urine in the later stages. With early diagnosis and appropriate treatment, prostate cancer is a disease that can be controlled and treated. Therefore, it is important for men to have regular health checks and be aware of risk factors.
WHAT ARE THE RISK FACTORS?
Prostate cancer risk factors are various factors that increase the likelihood of developing the disease. While some risk factors can be changed, others are beyond a person's control. The most important risk factors of prostate cancer:
Age: The risk of prostate cancer increases with age. Most cases occur in men over 50 years of age.
Family History: A person has a higher risk of developing this disease if a first-degree relative (father, brother) has prostate cancer.
Race/Ethnicity: Prostate cancer is more common in African American men and generally has a more aggressive course. It is less common in men of Asian descent.
Genetic Factors: Some genetic changes, especially BRCA1 and BRCA2 gene mutations, may increase the risk of prostate cancer.
Nutrition: High-fat diets and excessive consumption of red meat may increase the risk of prostate cancer.
Cigarette: Smoking may increase the risk of developing a more aggressive form of prostate cancer.
Obesity: It is thought that obesity may increase the risk of developing a more aggressive form of prostate cancer.
Environmental Factors: Some environmental factors, such as exposure to chemicals, can affect the risk of prostate cancer.
Hormone Levels: High levels of male hormones such as testosterone may affect the risk of prostate cancer.
Sedentary Lifestyle: Not being physically active may increase the risk of prostate cancer.
Each of these factors alone does not determine the risk of prostate cancer, but when considered together they can help understand the risk. Adopting a healthy lifestyle and regular health checks can be important steps in reducing the risk.
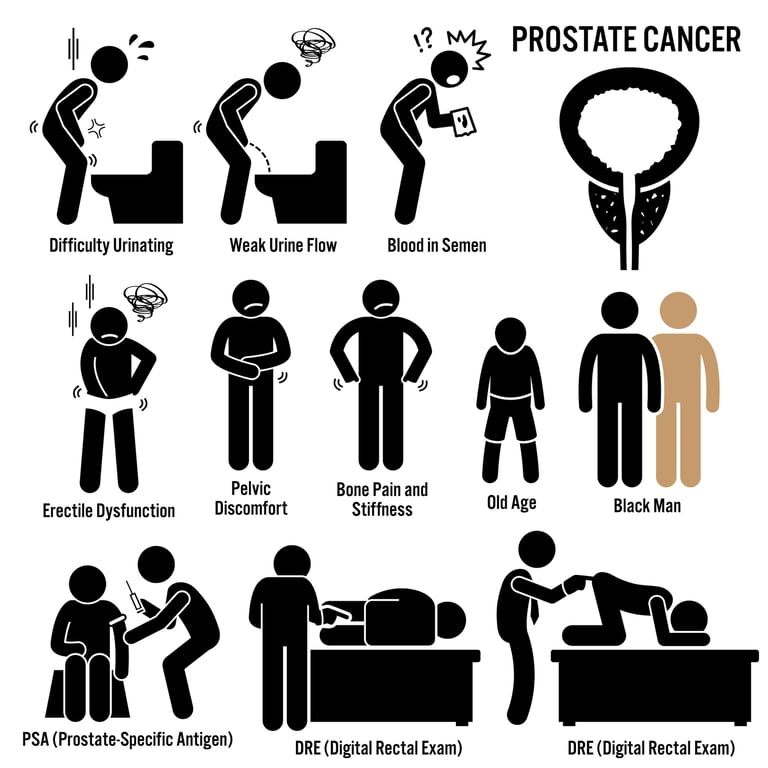
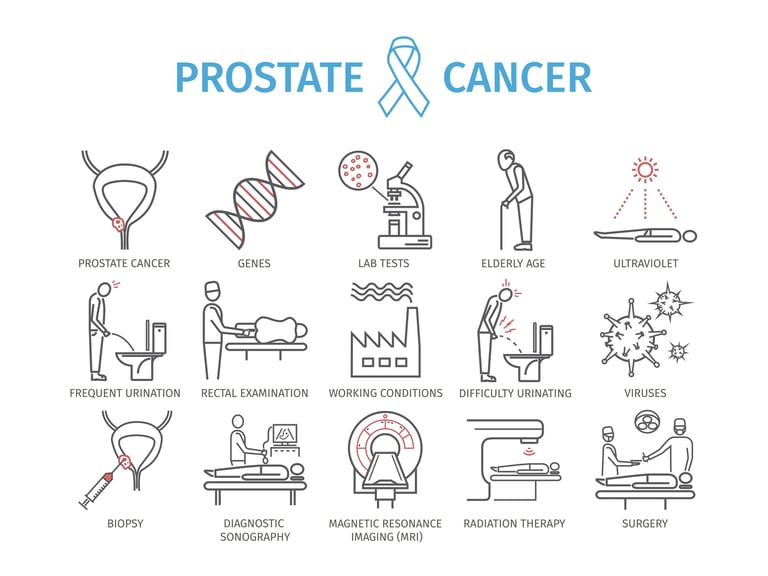
Image 1: Prostate cancer may cause complaints such as difficulty in urinating, decreased urine splashing force, and pain in the lower abdomen in elderly individuals.
HOW TO DEVELOP?
Prostate cancer is characterized by abnormal and uncontrolled cell growth in the cells of the prostate gland. The mechanisms of development of this type of cancer are complex and not fully understood, but a combination of genetic, environmental and hormonal factors are thought to play a role. Cancer development usually begins with DNA damage and genetic mutations. These mutations cause cells to divide and grow abnormally. Hormonal factors, especially androgens (male hormones), can affect the growth and proliferation of prostate cells, which can increase the risk of cancer. Additionally, family history and genetic predisposition may also play an important role; For example, some genetic changes, such as BRCA1 or BRCA2 gene mutations, may increase the risk of prostate cancer. Environmental factors and lifestyle choices, especially diet and physical activity levels, can also affect cancer development. However, there is an interaction of more than one factor in the development of prostate cancer, and the details of these interactions have not yet been fully resolved. Therefore, prostate cancer research continues to better understand the disease and develop effective treatment methods.
WHAT ARE THE SYMPTOMS?
Prostate cancer usually does not cause symptoms in its initial stages, but as the cancer grows or progresses, various symptoms may appear.
Common findings of prostate cancer:
Difficulty Urinating: Weakening of urine flow, intermittent urination or difficulty in starting to urinate may occur.
Need to Urinate Frequently: There may be a need to urinate frequently, especially at night.
Urgent Urinary Need: A sudden and violent need to urinate may be felt.
Blood in Urine or Sperm: There may be blood in the urine or semen.
Painful Urination or Ejaculation: There may be pain during urination or sexual intercourse.
Constant Pain in the Pelvic Region: There may be persistent pain or discomfort in the hip, pelvis or waist area.
Erection Difficulty: There may be an inability to achieve or maintain an erection sufficient for sexual intercourse.
Symptoms in Advanced Stages: As the cancer progresses, especially if it has spread to the bones, more serious symptoms such as bone pain may occur.
These symptoms do not always indicate the presence of prostate cancer and may be caused by other health conditions. However, it is important for men experiencing such symptoms to consult a physician. Early diagnosis plays a very important role in prostate cancer treatment.
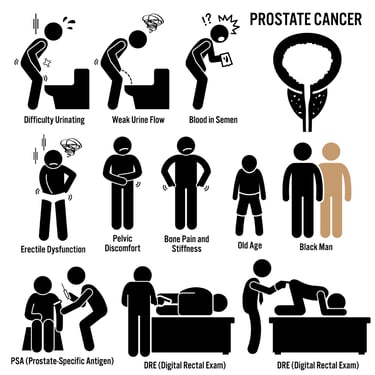
HOW IS IT DIAGNOSED?
The first step in diagnosing prostate cancer usually begins with a physical examination by a doctor, especially a rectal examination. During this examination, the doctor can detect abnormalities by feeling the size, shape, and texture of the prostate. Prostate-specific antigen (PSA) testing is another important tool for signs of cancer by measuring PSA levels in the blood; High PSA levels may indicate the possibility of prostate cancer but may not be definitive and may lead to false-positive results. If abnormalities are detected, a prostate biopsy is usually performed to make a more definitive diagnosis. During a biopsy, small samples of prostate tissue are taken and examined under a microscope for the presence of cancer cells. Imaging tests, such as transrectal ultrasonography (TRUS) or magnetic resonance imaging (MRI), can be used to view the prostate and surrounding tissues in more detail. These tests are used together to understand the presence, extent and spread of cancer and are critical in the diagnostic process. These diagnostic methods are vital for detecting prostate cancer at an early stage and determining appropriate treatment options.
WHAT ARE THE PATHOLOGICAL TYPES?
Prostate cancer is divided into several pathological types based on their histological features. These types are based on how cancer cells look under a microscope and how the cancer develops.
The most common pathological types of prostate cancer:
Adenocarcinoma: Most prostate cancers are adenocarcinomas. This type arises from the secretory cells of the prostate gland. Adenocarcinomas usually begin in the outer parts of the prostate and grow slowly.
Ductal Adenocarcinoma: This type, which originates from the duct structures of the prostate, may have a more aggressive course and is less common.
Müsinöz Adenocarcinoma: This type develops from mucus-producing cells and is a rare form of prostate cancer.
Small Cell Carcinoma: It is a very rare species and generally has a very aggressive course. Small cell carcinoma is the more common type of lung cancer, but it can also occur in prostate cancer.
Squamous Cell Carcinoma: It is a rare type of prostate cancer and originates from epidermal cells. This species generally follows a more aggressive course.
The pathological type of prostate cancer plays an important role in determining treatment options and prognosis. Therefore, it is critical to accurately evaluate the biopsy results and determine the type of cancer. The biological behavior and response to treatment of each species may be different. This information is used to create the most appropriate treatment plan for the patient.Some receptors and biological markers are critical in the treatment and diagnosis of prostate cancer. These receptors can influence the behavior of cancer cells and their response to treatment. Most importantly, androgen receptors (AR) play a central role in the development and progression of prostate cancer. Prostate cancer cells are often sensitive to androgens (male hormones, especially testosterone), and these hormones can promote the growth and spread of cancer cells. Therefore, hormone treatments often target androgen receptors and block the effects of these hormones or reduce androgen production. In some cases, tumor suppressor genes such as p53 and other molecular markers such as PTEN gene loss may also provide information about the aggressiveness and prognosis of prostate cancer. Understanding these receptors and markers helps better manage prostate cancer and plays an important role in the development of personalized treatment approaches.
Image 2: For the diagnosis of prostate cancer, PSA level, digital examination, MRI and biopsy are performed.

HOW IS TUMOR STAGING DONE?
Tumor staging in prostate cancer is done to determine the extent and degree of progression of the cancer. This process is used to understand the location of the cancer within the prostate, whether it has spread beyond the prostate and whether it has metastasized to other organs. Staging is usually done according to the following criteria:
TNM System: The TNM (Tumor, Nodal, Metastasis) system, which is widely used in the staging of prostate cancer, evaluates the size and extent of spread of the tumor (T), its spread to nearby lymph nodes (N) and whether there is metastasis to distant organs (M).
T Category (Tumor): Evaluates the size and local spread of the tumor in the prostate gland. They range from T1 to T4, with T1 representing the smallest local tumors and T4 representing large tumors that have spread to neighboring organs.
N Category (Nodal): Indicates whether the cancer has spread to regional lymph nodes. N0 means there is no cancer in the lymph nodes; N1 indicates cancer in the lymph nodes.
M Category (Metastasis): Indicates whether the cancer has spread to other parts of the body, such as bones or other organs. M0 means no distant metastasis; M1 indicates that there is metastasis.
Gleason Score: Gleason score is used to determine the extent of prostate cancer based on biopsy samples. This score evaluates how abnormal cancer cells look under a microscope. A score from 2 to 10 is obtained by adding the degrees of the two most common patterns. Higher Gleason scores indicate more aggressive cancer.
PSA Level: Prostate Specific Antigen (PSA) level measured by blood tests is also taken into account in prostate cancer staging. High PSA levels may indicate more advanced stage cancer.
This staging information helps doctors understand the extent of prostate cancer, determine treatment options, and evaluate the patient's prognosis. Each patient's situation is unique, and staging results form the basis of an individualized treatment plan.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Prostate cancer treatment varies depending on the stage of the cancer and requires a personalized approach. Treatment options are determined by taking into account the degree of spread of the cancer, the patient's general health condition and preferences. Here are general treatment approaches according to different stages of prostate cancer:
Stage I (Early Stage):
Active Monitoring: The cancer may be growing very slowly or not at all, so in some cases regular monitoring may be preferable rather than starting treatment immediately.
Radical Prostatectomy: It is the process of completely removing the prostate gland surgically.
Radiation Therapy: High-energy rays are used to destroy cancer cells.
Stage II (Locally Advanced Stage):
Radical Prostatectomy and sometimes removal of lymph nodes may be required.
Radiation Therapy can sometimes be used in conjunction with hormone therapy.
Hormone Therapy: Androgen deprivation therapy (ADT) blocks or reduces male hormones (androgens) that are necessary for the growth of cancer cells.
Stage III (Locally Advanced Cancer):
Radiation Therapy and Hormone Therapy are used together.
Radical Prostatectomy can be performed in some cases, but other treatment methods are generally preferred.
Stage IV (Metastatic Cancer):
Hormone therapy is used to slow the progression of cancer.
Chemotherapy; It can be especially applied to more aggressive cancer types that are resistant to hormone therapy.
New Generation Antiandrogen Therapies; It is used in metastatic disease.
Radiation Therapy or Surgery; It may be administered to relieve or control certain symptoms.
Supportive Care; Supportive treatments to manage pain and improve quality of life.
Treatment at each stage requires a detailed discussion and evaluation between the doctor and the patient to choose the most suitable one for the patient. Treatment decisions are personalized based on the patient's age, general health, characteristics of the cancer, and personal preferences. Regular follow-up and evaluation throughout the treatment process is also important because the course of the cancer and response to treatment may change.
Image 3: Prostate cancer is treated with surgery and radiotherapy in the early stages, and hormone-reducing drugs in the advanced stages.
WHAT ARE THE DRUGS USED IN TREATMENT?
There are various drugs and treatment methods used in the treatment of prostate cancer. These treatments may vary depending on the stage of the cancer, the patient's general health condition and the biological characteristics of the cancer.
The main types of treatment and drugs used in prostate cancer:
Chemotherapy
Docetaxel: Often used for metastatic prostate cancer.
Cabazitaxel: It is preferred in cases of resistant or previously treated metastatic prostate cancer.
Mitoxantrone: Used for pain management and improving quality of life.
Hormonal Therapies
LHRH (Luteinizing Hormone-Releasing Hormone) Analogues: Drugs such as Leuprolide, Goserelin, Triptorelin suppress testosterone production.
Antiandrogens: Drugs such as Bicalutamide, Flutamide, Enzalutamide block androgen receptors.
CYP17 Inhibitors: Abiraterone blocks androgen production by cancer cells.
GnRH Antagonists: Degarelix rapidly suppresses hormone production.
Smart Drug Therapies (Targeted Therapies)
PARP Inhibitors: Olaparib and Rucaparib are used in patients who carry BRCA mutations and meet certain criteria.
PSMA-Directed Therapies: Prostate-specific membrane antigen (PSMA)-directed radioligand therapies.
Immunotherapies
Sipuleucel-T: The first FDA-approved cancer vaccine is used especially in metastatic prostate cancer patients with minimal symptoms.
Checkpoint Inhibitors: Pembrolizumab is known as PD-1 or PD-L1 inhibitors and is used in the case of MSH-H.
Other Treatments
Radium-223: It is a radioactive treatment used in prostate cancer patients with bone metastases.
These medications and treatments are customized based on the patient's individual condition and response to treatment. During the treatment process, doctors and patients evaluate treatment options, taking into account the side effects of drugs, their effectiveness, and the patient's quality of life. The treatment plan is constantly reviewed and adjustments are made if necessary, depending on the nature of the cancer and the patient's general health condition.
HOW SHOULD FOLLOW-UP BE DONE AFTER RECOVERY?
Follow-up after recovery from prostate cancer is vital to reduce the risk of disease recurrence and provide early intervention. Follow-up usually begins with Prostate Specific Antigen (PSA) tests performed at regular intervals. Close monitoring of PSA levels provides early warning of the possibility of cancer recurrence. In addition, patients undergo regular physical examinations and, if necessary, rectal examinations. These examinations look for any signs of abnormality. For the first few years after treatment, PSA testing is usually done every three to six months. As the risk of cancer recurrence decreases over time, the frequency of these tests may be reduced. Additionally, regular follow-ups are performed to manage side effects of treatment and optimize overall health. During these follow-ups, counseling can also be provided on issues such as lifestyle changes, nutrition and exercise. If the patient has any new symptoms or concerns, these should be reported to their healthcare provider immediately. A comprehensive follow-up program helps protect the patient's health and maximize quality of life.