Penile Cancer
21.03.2025
PENIS CANCER DIAGNOSIS AND TREATMENT


Penile cancer is a type of cancer that occurs as a result of uncontrolled growth and proliferation of penile cells. It usually begins in the skin or inner tissue of the penis. Penile cancer is a rare type of cancer worldwide, but it can lead to serious consequences. Early diagnosis and treatment increases the chance of success. The important thing is for men to pay attention to their genital health and not neglect abnormal symptoms (for example, lesions, swelling or bleeding). Risk factors may include smoking, HPV infection, lack of sexual hygiene, and genetic factors. While penile cancer can be treated in the early stages, when it spreads in advanced stages, more complex and challenging treatment may be required. Therefore, it is important for men to have regular health checks and be aware of sexual health issues.
WHAT ARE THE RISK FACTORS?
Penile cancer risk factors may include:
HPV Infection: The virus called Human Papillomavirus (HPV) may increase the risk of penile cancer. Especially HPV types 16 and 18 may be effective in the formation of this cancer.
Smoking: Smoking may increase the risk of penile cancer. The chemicals in cigarette smoke can damage penile cells.
Phimosis: Phimosis is a condition in which the skin of the penis becomes tightly covered and can make it difficult to clean the glans. This can increase the risk of infection due to lack of cleanliness.
Age: Penile cancer is generally more common in men over the age of 60.
Hygiene: Lack of sexual hygiene may increase the risk of penile cancer.
Family History: Family history may increase the risk of penile cancer.
Paraphimosis: Paraphimosis is a condition in which a stuck glans cannot be pulled back and can increase the risk of infection.
Other Sexually Transmitted Infections:Other sexually transmitted infections may also increase the risk of penile cancer.
These risk factors can affect a person's risk of developing penile cancer, but even if a person has these factors, the likelihood of developing the cancer may be low. Additionally, the effects of risk factors can be reduced with measures such as healthy lifestyle choices and regular doctor check-ups.
Image 1: Penile cancer occurs from cells in the skin or inner layer of the penis along the penis line.
HOW DOES IT OCCUR?
The mechanisms of development of penile cancer involve a complex network of interactions and are not fully understood. However, some potential factors and mechanisms may be: Human Papillomavirus (HPV) infection may increase the risk of penile cancer. Some types of HPV can cause abnormal changes in penile cells. Smoking may increase the risk of penile cancer; There is a possibility that carcinogenic substances in cigarette smoke may damage penile tissues. Lack of hygiene and sexually transmitted infections can affect the development of penile cancer. The combination of these factors can lead to DNA damage in penile cells and ultimately contribute to the formation of cancer cells. However, the exact development mechanisms of penile cancer are still a matter of research and more studies are required.
WHAT ARE THE SYMPTOMS?
Symptoms of penile cancer may include:
Painless Wounds or Lesions on the Penis: There may be significant sores, ulcers, nodules or lesions on the penis. These lesions are usually painless.
Color Changes: Abnormal color changes or skin rashes may occur on the penis.
Swelling in the Penis:There may be a swelling or swollen feeling in one area of the penis.
Urinary Tract Problems: Difficulty urinating, change in urine flow, changes in urine color, or bloody urine may occur.
Inflammation and Pain: Symptoms such as inflammation, pain or itching around the penis may occur.
These symptoms may occur in the early stages of penile cancer. If such symptoms are experienced or any abnormality in sexual health is noticed, a urologist should be consulted. Early diagnosis can increase treatment success and improve treatability.
HOW IS IT DIAGNOSED?
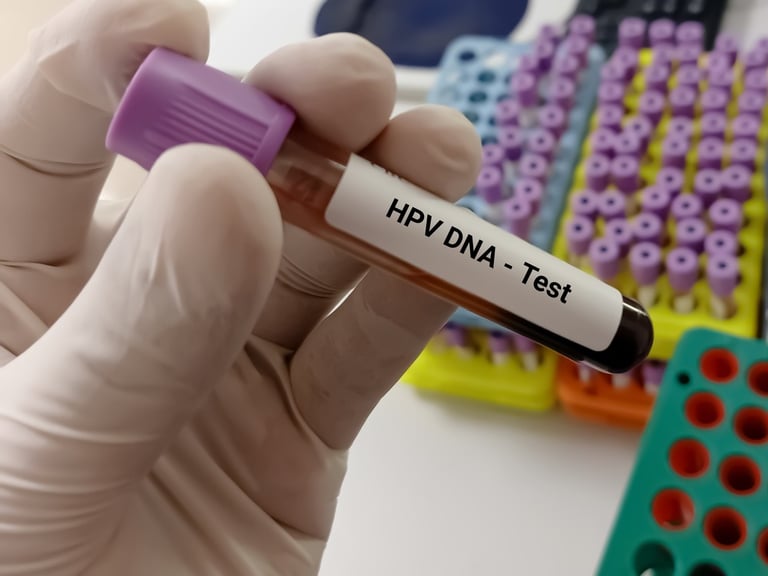
Diagnosis of penile cancer usually begins upon noticing suspicious symptoms or abnormal findings. The diagnostic process may include physical examination, biopsy and imaging methods. The doctor begins by examining lesions or abnormal areas on the penis. Then, samples of the suspicious tissue are taken in a procedure called biopsy and these samples are sent for laboratory examination. Biopsy results confirm or deny the presence of cancer cells. Imaging methods can be used to evaluate the spread of cancer. The diagnostic process is individualized depending on the patient's symptoms, risk factors, and findings. Early diagnosis can increase treatment success, so it is important to contact a healthcare professional if experiencing any abnormal signs or symptoms.
WHAT ARE THE PATHOLOGICAL TYPES?
Pathological types of penile cancer can be:
Squamous Cell Carcinoma: The majority of penile cancers arise from squamous cell carcinoma. This type of cancer can occur on the skin or inner surface of the penis.
Squamous Cell Papilloma: Squamous cell papillomas are a less aggressive type of squamous cell carcinoma and are considered a benign (non-malignant) tumor.
Adenocarcinoma: This type of cancer originates from the glandular cells of the penis. Adenocarcinoma is not as common as squamous cell carcinoma, but can occur in rare cases.
Basal Cell Carcinoma: This type of cancer originates from the skin cells of the penis and is usually not as aggressive as other types of cancer.
Each pathological type may reflect the characteristics and behavior of cancer differently. Treatment options are determined depending on the type of cancer, its stage and the patient's general health condition. Pathological examination helps to make a correct diagnosis and create an appropriate treatment plan.R eceptors important in penile cancer are used to understand the biological characteristics of cancer and response to treatment. These receptors include factors such as the Epidermal Growth Factor Receptor (EGFR), the Androgen Receptor, which regulates hormonal effects, PD-L1 and PD-1, which help determine response to immunotherapy, HER2, which indicates aggressiveness in some species, and Ki-67, which indicates cell division rate. Assessing these receptors may help personalize penile cancer treatment and help patients receive more effective treatment.
Image 2: HPV virus is an important factor in the development of penile cancer.

HOW IS TUMOR STAGING DONE?
Staging of penile cancer is used to determine the spread and severity of the disease. Penile cancer staging is usually done by the following methods:
Physical Examination: The doctor examines the penis and surrounding area to evaluate the presence of penile cancer and the size of the tumor.
Computed Tomography (CT) or Magnetic Resonance Imaging (MRI): These imaging methods help visualize the size of the tumor and surrounding tissues in more detail. It can also be used to evaluate whether it has spread to lymph nodes or other organs.
Lymph Node Biopsy: If penile cancer tends to spread, nearby lymph nodes may be biopsied.
Cystoscopy: This is an invasive procedure and is used to evaluate the presence and stage of the tumor. A flexible tube (cystoscope) is inserted into the penis and the doctor can observe the tumor and perform a biopsy.
Penile cancer staging is done by combining information used to determine the stage of the disease. Based on this information, a classification established by the American Cancer Society is used. Staging is important in determining the stage and spread of cancer and helps determine appropriate treatment options.
Staging of penile cancer is used to determine the extent and severity of the disease. This staging process usually includes the following stages:
Stage I: At this stage, the cancer is limited only to the upper layers of the penis and has not spread to other tissues. The tumor is usually small in size.
Stage II: The cancer has spread to the deeper tissues of the penis, but has not yet spread to other surrounding organs or lymph nodes.
Stage III: At this stage, the cancer has spread to the deep tissues of the penis, lymph nodes, or nearby tissues.
Stage IV: At this stage, the cancer has spread to organs other than the penis or to distant areas (e.g., lungs, liver). Stage IV refers to metastatic cancer.
The staging process is supported by physical examination, imaging studies (CT, MRI), lymph node biopsy and other diagnostic tests. Staging results play an important role in determining a patient's cancer treatment plan and predicting prognosis. Therefore, accurate staging is vital for determining appropriate treatment options.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Penile cancer treatment may vary depending on the stage of the disease and the extent of spread. The treatment plan may include different treatment methods such as:
Stage 0: In the early stage of penile cancer, the tumor is limited only to the surface of the skin. In this case, treatment options usually include removing the tumor. Such treatments may also include minimally invasive methods such as electrocautery or laser surgery.
Stage I and II: In these stages, the tumor may have spread to deeper tissues, but has not spread to lymph nodes or other organs. Treatment options may include surgery (penectomy or glans resection), radiotherapy, or combination treatments. Depending on whether lymph nodes are involved, removal of the lymph nodes may also be necessary.
Stage III: Stage III penile cancer has spread to peripheral tissues or lymph nodes. Treatment usually involves more extensive surgical removal. Lymph nodes may also be involved and radiotherapy may also be considered. In some cases, chemotherapy is also added.
Stage IV: At this stage, the cancer has spread to organs other than the penis or to distant areas (e.g., lungs, liver). Treatment is more complex and can often include systemic chemotherapy, targeted therapies, and immunotherapy. Surgery may often be inadequate to treat cancer that has spread.
Treatment options are personalized based on factors such as the patient's medical condition, age, general health, and response to treatment. The treatment plan is determined by an oncologist or urologist and can be adjusted according to the patient's condition. Early diagnosis and appropriate treatment can increase the chances of success in treating penile cancer.
Image 3: People with persistent wounds in the penis area should consult a urologist.


WHAT ARE THE SYSTEMIC DRUGS USED IN TREATMENT?
Various medications and treatment options used to treat penile cancer may include:
Chemotherapy:
Cisplatin: It is a chemotherapy drug frequently used in penile cancer.
5-Fluorouracil (5-FU): Can be used together with cisplatin.
Paclitaxel: May be included in chemotherapy regimens.
Immunotherapy:
Pembrolizumab and nivolumab: Immunotherapy drugs stimulate the immune system to attack cancer cells and can be used to treat penile cancer. Immunotherapy has been an area of interest in the treatment of penile cancer in recent years and may be effective in some cases.
Treatment options are determined depending on the patient's stage, biological characteristics of the tumor and general health status. The treatment plan is created individually by an oncologist or urologist. It is important for patients diagnosed with penile cancer to carefully consider their treatment options and risks.
HOW SHOULD FOLLOW-UP BE DONE AFTER RECOVERY?
Follow-up after treatment for penile cancer is important to monitor the patient's health and assess the risk of cancer returning or developing other complications. The follow-up plan is personalized based on the patient's treatment history, stage of cancer, and treatment response. It often may include: regular doctor exams, blood tests, imaging studies (for example, CT or MRI). During follow-up, the patient's symptoms, side effects and quality of life are also evaluated. Early diagnosis and monitoring response to treatment can improve a patient's long-term health outcomes and enable intervention when necessary. The post-treatment follow-up plan should be implemented meticulously in order to best protect the patient's health.