Osteosarcoma
21.03.2025
OSTEOSARCOMA DIAGNOSIS AND TREATMENT
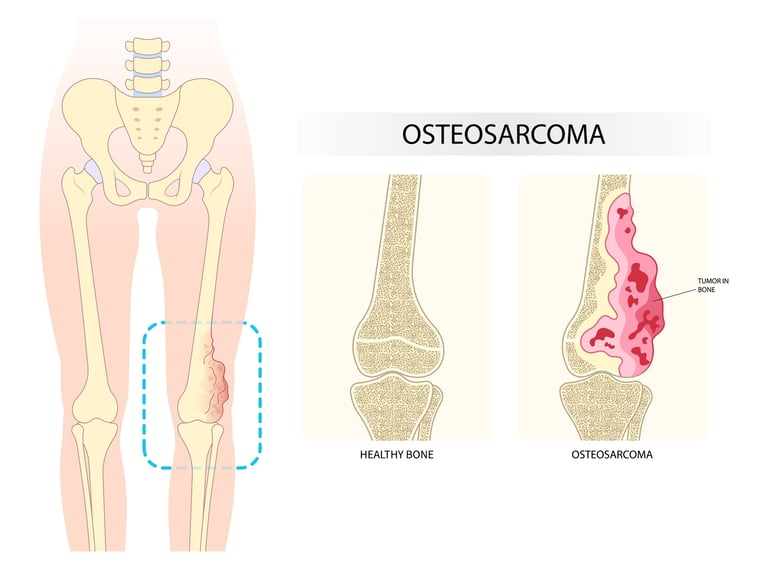
Osteosarcoma is the most common type of bone cancer, especially among young adults and children, and usually occurs in the growth areas of long bones, such as the thigh and shin bones near the knees. This type of cancer originates from bone-forming cells (osteoblasts) and can grow aggressively and spread to surrounding tissues and other organs (especially the lungs). The importance of osteosarcoma stems from the fact that it is an important cause of cancer in young individuals and that it can progress rapidly and become life-threatening if left untreated. Treatment usually includes surgery and chemotherapy, and early diagnosis can significantly increase treatment success. Thanks to advanced treatment methods, the survival rates of patients with osteosarcoma have improved significantly in recent years. However, the aggressive nature of the disease and the fact that it usually affects young individuals requires continued research and advancements in the diagnosis and treatment of osteosarcoma. Increasing awareness of this type of cancer, early diagnosis and development of effective treatment strategies are vital.
WHAT ARE THE RISK FACTORS?
Although the exact cause of osteosarcoma is not always clear, some factors are known that may increase the risk of developing this type of cancer.
Known risk factors of osteosarcoma:
Age and Gender: Osteosarcoma is usually seen in young people during adolescence and rapid bone growth occurs during this period. It is slightly more common in boys than girls.
Familial Genetic Diseases: Some genetic disorders, especially diseases such as Li-Fraumeni syndrome, Rothmund-Thomson syndrome, and sometimes retinoblastoma, may increase the risk of osteosarcoma.
Radiation Therapy: High-dose radiation therapy, especially when given at a young age, may increase the risk of osteosarcoma in later years.
Paget's Disease: This disease is usually seen in older adults and causes bones to grow abnormally. People with Paget's disease may have an increased risk of osteosarcoma, but this condition is rare.
Rapid Growth in Long Bones: Rapid growth of long bones during adolescence has been associated with the development of osteosarcoma.
Some Metal Implants: In very rare cases, metal bone implants may increase the risk of osteosarcoma.
Each of these risk factors can increase the risk of developing osteosarcoma, but most cases of osteosarcoma have no specific cause. Especially people with genetic risk factors or previous radiation therapy are recommended to reduce their risks through regular medical follow-up and check-ups. Individuals with a family history or other risk factors should consult their doctor for medical advice and early diagnosis.
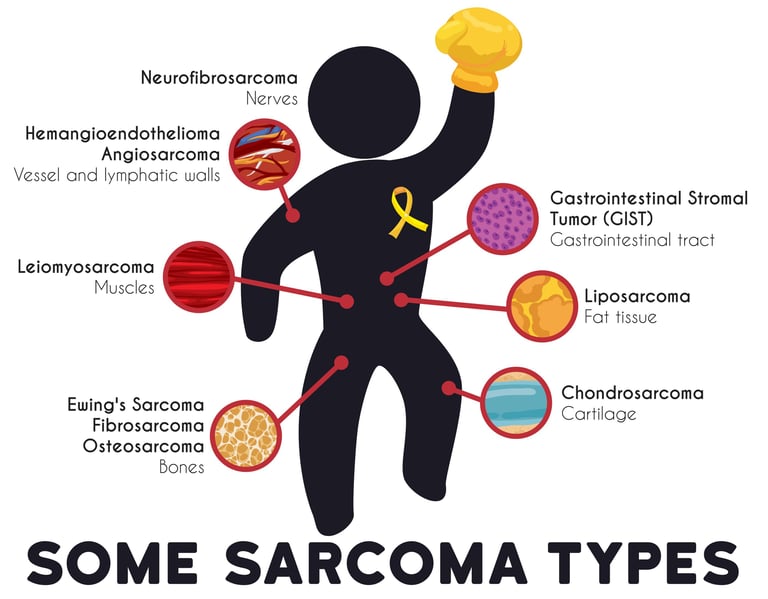
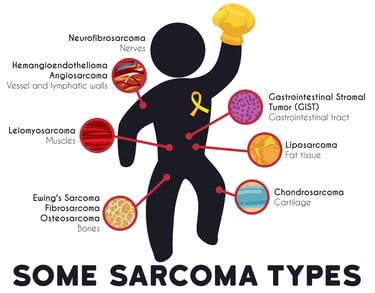
Image 1: Sarcomas can occur from connective tissues and bone tissues.
HOW DOES IT OCCUR?
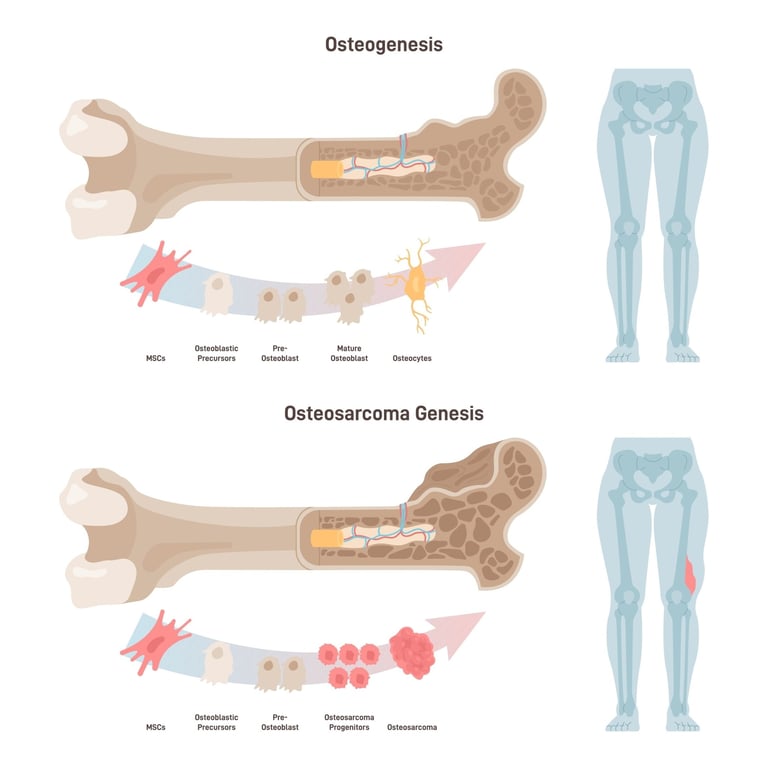
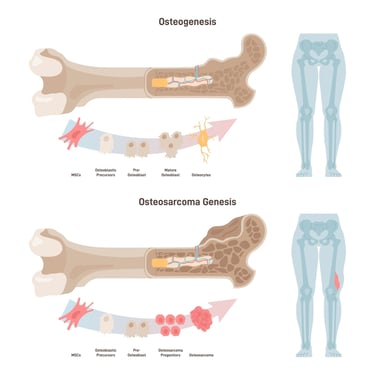
Although the mechanism of development of osteosarcoma is complex and not fully understood, it is mainly characterized by abnormal and uncontrolled growth of bone-forming cells (osteoblasts). In this type of cancer, mutations in the cells' DNA lead to dysfunction of genes that regulate normal cell growth and death. These genetic changes cause cells to overgrow and produce abnormal bone or bone-like material instead of normal bone tissue. In some cases, these mutations can be associated with genetic diseases, radiation exposure, or other environmental factors, but in most cases a specific trigger cannot be identified. Osteosarcoma usually develops in the growth areas of bones, especially at the ends of long bones (for example, near the knee), indicating that cells in the process of growth are particularly susceptible to this type of cancer. They are constantly conducting studies at the genetic and molecular level to better understand the mechanisms of development of osteosarcoma, which may lead to the development of more effective treatment methods in the future.
WHAT ARE THE SYMPTOMS?
Symptoms of osteosarcoma can vary depending on the size, location, and spread of the cancer, but some common findings include:
Pain: The most common symptom is pain in the affected bone area. Initially, the pain is usually mild and intermittent, but over time it can become constant and severe. Pain may be exacerbated by physical activity or at night.
Swelling or Mass: Swelling or a mass may be noticed in the affected bone area. This swelling can grow over time and is often painful.
Movement Restriction: If the tumor is located near a joint, movement limitation or discomfort may occur in that joint.
Fractures: In some patients with osteosarcoma, the affected bone may weaken and lead to unexpected fractures even during normal activities.
Fatigue and Weakness: Fatigue and weakness may occur due to the deterioration of general health status and the effect of cancer on the body.
Weight Loss: In advanced cases, patients may experience unexplained weight loss.
Fever and Sweating: Some patients may experience fever and sweating, especially at night.
Osteosarcoma symptoms can be confused with other more common conditions (for example, sports injuries), so if you have any of these symptoms, especially if they persist for a long time, it is important to see a doctor for a medical evaluation. Early diagnosis is critical for the effectiveness of treatment.
HOW IS IT DIAGNOSED?
Diagnosing osteosarcoma usually involves a series of steps, and the process begins with the patient's symptoms and medical history. First, the doctor performs a physical examination and evaluates the patient's symptoms, pain, swelling, and any loss of function. In case of doubt, imaging tests are performed to confirm the diagnosis; these include x-rays, magnetic resonance imaging (MRI), and computed tomography (CT) scans. These tests help determine the tumor's location, size, and effect on surrounding bones or tissues. For definitive diagnosis, a tissue sample is taken from the affected area and a biopsy is performed. This sample is examined under a microscope and the presence and type of cancerous cells are determined. If necessary, additional imaging tests (for example, PET scan) and bone scans may be performed to determine the extent and stage of the tumor. This comprehensive evaluation is critical to determine the type and stage of osteosarcoma and appropriate treatment options. Once a diagnosis of osteosarcoma is made, a multidisciplinary approach is taken for treatment planning, a process usually managed by a team consisting of medical oncologists, orthopedic surgeons, and radiation oncologists.
WHAT ARE THE PATHOLOGICAL TYPES?
Osteosarcoma can be divided into several pathological subtypes, each with different microscopic features. These subtypes are classified based on the appearance of the tumor cells and the type of material they produce.
Some common pathological types of osteosarcoma:
Conventional Osteosarcoma: It is the most common type of osteosarcoma and usually involves malignant cells within the bone that produce osteoid (bone material). This type usually occurs in young adults and children.
Chondroblastic Osteosarcoma: This type contains cells that produce cartilage-like material. Under the microscope, it shows cartilage-related features.
Fibroblastic Osteosarcoma: In this type, part of the tumor consists of fibrous (connective tissue) material. Cells generally show a more ordered structure.
Telangiectatic Osteosarcoma: This rare species often contains large, blood-filled cavities. It may have an aggressive appearance under the microscope.
Small Cell Osteosarcoma: This type contains small, round, blue cells and looks like other small cell tumors under a microscope.
Periosteal (Juxtacortical) Osteosarcoma: It is a low-grade tumor that grows on the bone surface. It usually occurs in adults and has a better prognosis.
High Grade Superficial Osteosarcoma: It is a rare species that grows on the bone surface and shows high-grade malignant features.
Each of these pathological types differs in how the disease is treated and its prognosis. Determining the pathological type of the tumor during the diagnosis process is important for treatment planning and is usually done by detailed pathological examination of the biopsy sample.In pathological examinations of osteosarcoma, histopathological findings and biopsy results are more important than the receptors that should be taken into consideration. Osteosarcoma is evaluated in detail by pathologists, especially during the examination of malignant tumors in bone tissue. Pathological examination identifies abnormalities in bone tissue, morphological features and cellular characteristics of the tumor. The presence of osteoid production is especially important for the diagnosis of osteosarcoma, as this is the main feature of the tumor. However, pathological examination also provides information about the aggressiveness and stage of the tumor. Advanced techniques such as genetic studies and immunohistochemistry can also be used, but definitive diagnosis and evaluation are usually based on histopathological findings. The treatment plan for osteosarcoma is determined based on the results of pathological evaluation, and therefore pathologists play a critical role in accurately understanding the disease.
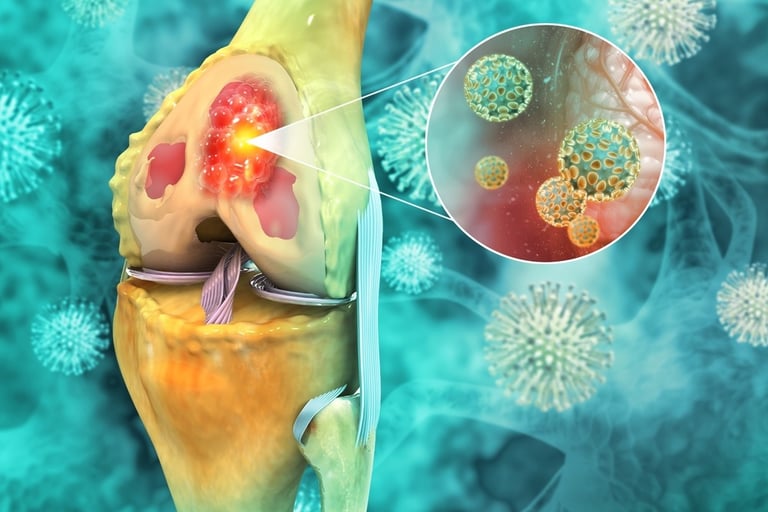
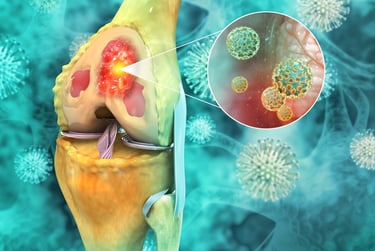
Image 2: Osteosarcoma often occurs in the knee area.
HOW IS TUMOR STAGING DONE?
Staging of osteosarcoma is an important step to determine the extent of tumor spread and the treatment plan. Staging of osteosarcoma is usually done by the following methods:
Physical Examination: The patient's general health condition and the location of the bone tumor are evaluated by physical examination.
Imaging Tests:
X-ray: The size, shape of the bone lesion and changes in the bone tissue are examined by x-ray.
Magnetic Resonance Imaging (MRI): MRI shows the spread of the tumor within the bone and surrounding tissues in more detail.
Computed Tomography (CT): CT scans are used to more clearly see the details of the tumor within the bone.
Bone Scintigraphy: Bone scintigraphy is used to evaluate the risk of tumor spread to other bones.
Biopsy: The diagnosis of osteosarcoma is confirmed by biopsy. The biopsy sample is examined by pathologists and provides information about the type and aggressiveness of the tumor.
Staging: Staging of osteosarcoma is usually done according to the TNM (Tumor, Lymph Node, Metastasis) system. This system evaluates tumor size (T), spread to lymph nodes (N), and the presence of distant metastases (M). Based on the staging results, the stage of the disease is determined (for example, stage I, II, III or IV) and an appropriate treatment plan is created.
Advanced Imaging and Laboratory Tests: During the staging phase, advanced imaging methods such as PET scans or bone scans may be used. Additionally, laboratory tests such as blood tests and bone marrow aspirate may be used to evaluate metastases or tumor activity.
Staging of osteosarcoma is a critical step in determining the patient's treatment plan and predicting prognosis. Treatment options may often include surgery, chemotherapy, and radiotherapy, depending on the stage of the tumor. Therefore, accurate staging is important and should be done carefully by the patient's healthcare team.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Osteosarcoma treatment may vary depending on the stage and grade of the tumor.
Here are the treatment approaches for osteosarcoma according to stages:
Stage I: Stage I osteosarcomas are usually locally limited and have not spread to peripheral tissues. Treatment usually begins with surgical excision. A prosthesis or graft can be used to remove the tumor and fill the gap in the bone. Chemotherapy is often used to prevent the spread and recurrence of tumor cells.
Stage II: Stage II osteosarcomas may have spread further into peripheral tissues. Treatment again begins with surgical excision, but in this case the size and spread of the tumor is more important. Before or after surgery, chemotherapy is often used to kill tumor cells and reduce the risk of recurrence.
Stage III: Stage III osteosarcomas have spread to peripheral tissues and lymph nodes. Treatment includes surgical excision, but surgery may cover a larger area. In advanced stages, chemotherapy is often given before and after surgery, and sometimes radiotherapy may also be required.
Stage IV: Stage IV osteosarcomas have metastasized to distant organs. Treatment is usually managed much more aggressively. Surgical intervention aims to remove as much of the tumors as possible. Chemotherapy is at the center of treatment and includes treatment for all areas that have metastasized. Radiotherapy may be used to relieve or control symptoms.
Treatment for osteosarcoma may vary depending on the stage of the tumor and the patient's overall health. The treatment plan must be determined by a multidisciplinary healthcare team and may include a combination of surgery, chemotherapy, and radiotherapy. The treatment process is closely monitored to manage the patient's side effects and monitor his or her health. The patient's individual condition and response to treatment are also important and the treatment plan can be adapted as necessary. Osteosarcoma treatment is a complex process and should be guided by expert advice.
Image 3: Osteosarcoma It is characterized by abnormal and uncontrolled growth of bone-forming cells (osteoblasts).
WHAT ARE THE SYSTEMIC DRUGS USED IN TREATMENT?
Chemotherapy, smart drug treatments and immunotherapies used in the treatment osteosarcoma may include:
Chemotherapy drugs:
Methotrexate: It is a chemotherapy drug frequently used in the treatment of osteosarcoma. It neutralizes tumor cells by preventing them from growing and multiplying.
Cisplatin: It is another common chemotherapy drug and works by killing tumor cells.
Doxorubicin: It is an anthracycline chemotherapy drug used in the treatment of osteosarcoma. It targets and inhibits tumor cells.
Ifosfamide: It is another chemotherapy agent used in the treatment of osteosarcoma. It targets tumor cells and prevents them from growing.
Smart Drug Therapies (Targeted Therapies):
Targeted drugs used in the treatment of osteosarcoma (bone cancer) aim to prevent the growth and spread of these cells by targeting the special features of cancer cells. Such treatments can be used as an alternative or complement to traditional chemotherapy.
Sorafenib: It is a multi-kinase inhibitor and can restrict the growth and spread of cancer cells by blocking the process of angiogenesis (formation of new blood vessels).
Regorafenib: Similar to sorafenib, this drug works to stop the growth and spread of osteosarcoma cells by blocking the angiogenesis process.
Pazopanib: Another multi-kinase inhibitor, pazopanib may help inhibit the growth of cancer cells by targeting various tyrosine kinases.
These drugs are generally used in advanced stages of osteosarcoma or in cases that are resistant to standard treatments. The effectiveness of targeted therapies may vary depending on the genetic characteristics of the cancer and the individual response of the patient. When deciding on treatment options and medication use, an oncologist's opinion should be obtained. Since the use and effectiveness of these medications may vary from patient to patient, treatment planning should be individualized.
Immunotherapies:
The use of immunotherapies in the treatment of osteosarcoma is limited and further studies are required. Immunotherapy can be used to stimulate the immune system to recognize and target tumor cells.
Treatment for osteosarcoma may vary depending on the patient's stage, the genetic make up of the tumor, and other individual factors. The treatment plan should be determined by an oncologist and customized to suit the patient's condition. Therefore, treatment options and medications may vary depending on the patient's specific condition and should be consulted with a medical professional.
HOW SHOULD FOLLOW-UP BE DONE AFTER RECOVERY?
Follow-up after osteosarcoma treatment is important to monitor the patient's recovery progress and to detect possible recurrence or post-treatment complications early. Post-recovery follow-up may include regular doctor exams, imaging tests (for example, X-rays, MRIs, or CT scans), blood tests, and bone scintigraphy. Frequency of follow-up may vary depending on the stage of the disease, response to treatment, and the patient's individual risk factors. Post-treatment follow-up may also include physical therapy and psychosocial support to assess rehabilitation needs and improve quality of life. Post-recovery follow-up plays a vital role in maintaining the patient's long-term health and quality of life, and this process should be conducted in close collaboration with the patient's oncologist.