Oropharyngeal Cancer
21.03.2025
OROPHARYNX CANCER DIAGNOSIS AND TREATMENT


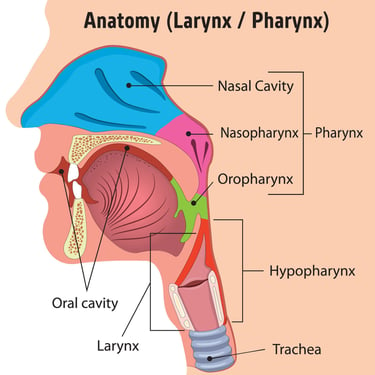
Oropharynx cancer is a type of cancer that develops in the back of the oral cavity, in the pharynx (oropharynx) region. The oropharynx includes the base of the tongue, tonsils, soft palate, and the back of the throat. This type of cancer is often associated with infections caused by a virus called HPV (Human Papillomavirus). HPV-related oropharyngeal cancer is more common in young, healthy individuals and generally has a better prognosis. However, non-HPV oropharyngeal cancer also exists and may have a different etiology. Oropharynx cancer can be treated when diagnosed early, but when diagnosed in advanced stages, treatment may become difficult and may lead to more serious consequences. Therefore, regular health checks and preventive measures such as vaccinations are important in reducing the risk of oropharynx cancer. Oropharyngeal cancer is a type of cancer whose symptoms require attention, and early diagnosis and treatment can improve patients' quality of life and improve their chances of survival.
WHAT ARE THE RISK FACTORS?
Risk factors that are effective in the development of oropharynx cancer may be:
HPV Infection (Human Papillomavirus): HPV, especially high-risk types such as HPV types 16 and 18, is one of the main causes of oropharynx cancer. This sexually transmitted virus can infect the oral and throat mucosa.
Cigarettes and Tobacco Products: Smoking or using tobacco products may increase the risk of mouth and throat cancers. The risk of HPV-positive people who smoke may be even higher.
Excessive Alcohol Use: Excessive alcohol consumption may increase the risk of oropharynx cancer. The risk increases even more when alcohol and smoking come together.
Sexual Intercourse Behaviors: People who have multiple sexual partners or are sexually active have a higher risk of HPV infection.
Age: Oropharynx cancer is generally more common in individuals over the age of 40.
Male Gender: It is known that the risk of oropharynx cancer is higher in men than in women.
Genetic Factors: A family history of cancer or certain genetic factors may increase the risk.
Immune System Weakness: People with weakened immune systems may be more vulnerable to HPV infections.
Oral Hygiene and Dental Problems: Poor oral hygiene or gum problems can promote the long-term presence of oral sores and increase the risk of cancer.
Asbestos and Dust Exposure: Occupational exposure, especially to harmful substances such as asbestos and dust, can increase the risk of oropharynx cancer.
These risk factors can affect the development of oropharyngeal cancer, but everyone's risk of developing cancer is different. In particular, the fact that HPV infection is associated with oropharynx cancer makes the development of this cancer even more complicated. Preventive measures and regular health checks can reduce the risk and support early detection of cancer.
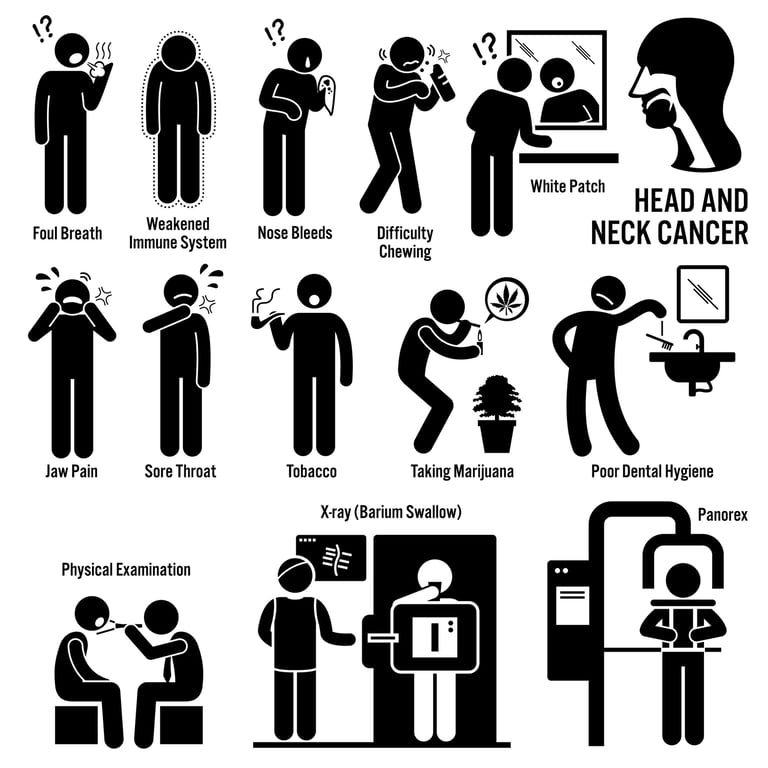
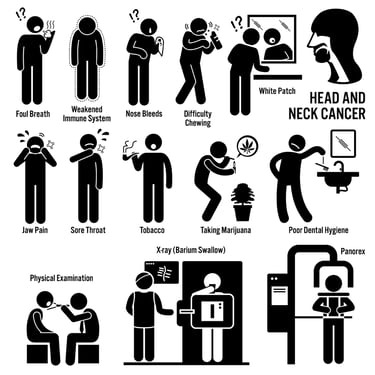
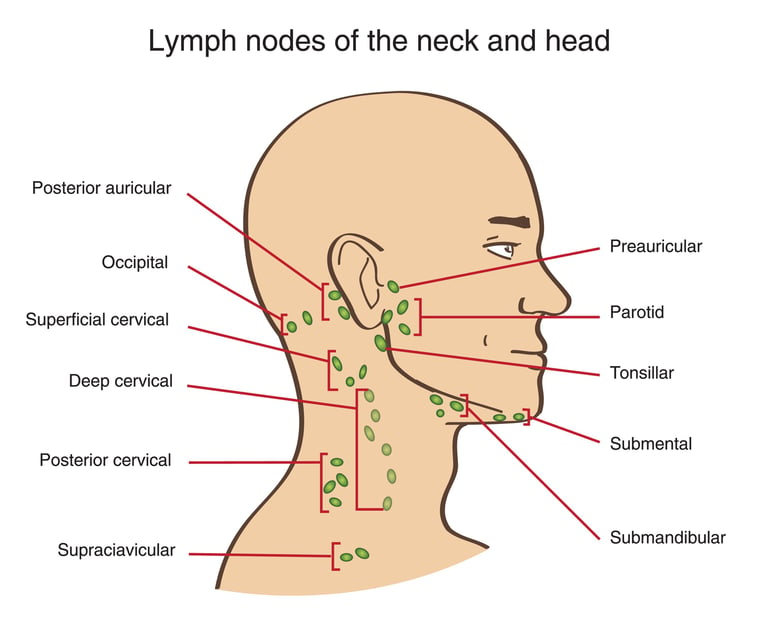
Image 1: Sore throat, swelling and swallowing problems may occur due to oropharynx cancer.
HOW DOES IT OCCUR?
The mechanisms of development of oropharyngeal cancer are related to complex interacting factors. HPV (Human Papillomavirus) infection is one of the most important causes of oropharynx cancer. HPV can settle in the mucosa of the mouth and throat and cause genetic changes in the cells. Particularly high-risk HPV types play a critical role in cancer formation. In addition to HPV, smoking, use of tobacco products, and excessive alcohol consumption may increase the risk of oropharynx cancer. These factors can contribute to mutations in cellular DNA, changes in genes that control cellular growth and division, and the formation of cancer cells. Oropharyngeal cancer development mechanisms result from the complex interaction of genetic, environmental and virus-related factors, and therefore, fully understanding and controlling this disease requires a challenging process.
WHAT ARE THE SYMPTOMS?
Symptoms of oropharynx cancer may vary from person to person and depend on the stage, type, and extent of spread of the cancer. Symptoms of oropharynx cancer may include:
Painless Swallowing Difficulty: Pain or difficulty may be experienced while swallowing.
Sore throat:There may be a feeling of chronic or recurring sore throat.
Enlargement of Tonsils: Oropharynx cancer can cause enlargement of the tonsils.
Pain During Swallowing: There may be pain or discomfort when eating or consuming liquids.
Earache: Earache can occur if cancer has spread to or around the ear canal.
Shortness of breath: As the cancer grows or spreads, there may be a feeling of shortness of breath.
Voice Changes: Hoarseness or changes in voice may be observed.
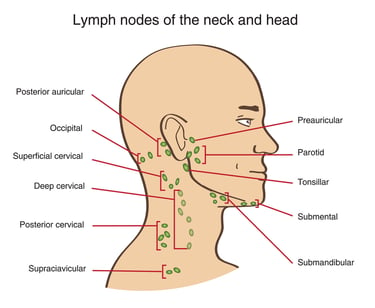
Swellings on the Neck: It is possible for lymph nodes to swell in the neck or to feel palpable masses.
Bloody Saliva: Bloody saliva or bloody sputum may occur.
Intraoral Lesions: There may be sores, lesions or white spots in the mouth or throat.
An important point to remember is that these symptoms alone do not mean oropharynx cancer. However, if such symptoms are present, it is important to be evaluated by a physician. Early diagnosis can increase cancer treatment success.
HOW IS IT DIAGNOSED?
Oropharyngeal cancer is diagnosed using a series of medical tests and imaging studies. The first step is a physical examination by an ear-nose-throat (ENT) specialist or oncologist and a detailed evaluation of the patient's symptoms and history. Other methods used for diagnosis may include:
Endoscopy: The inside of the mouth and throat are visually examined using a fiberoptic endoscope. This may help detect cancerous lesions.
Biopsy: Tissue samples are taken from suspicious lesions and sent to the laboratory for pathological examination. The biopsy result helps determine the type and stage of cancer.
Imaging Tests: Imaging tests such as computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) are used to evaluate the spread and stage of cancer.
Lymph Node Biopsy: If the cancer has spread, tissue samples can be taken from the lymph nodes in the neck to determine how far the cancer has progressed.
Diagnosing oropharyngeal cancer requires a multidisciplinary approach and may involve the collaboration of many different specialists. Early diagnosis can help treat oropharyngeal cancer successfully, so it is important for people with any suspicious symptoms or risk factors to see a doctor.
WHAT ARE THE PATHOLOGICAL TYPES?
Oropharyngeal cancer can be of different pathological types, and these types define the cellular structure and behavior of the cancer.
Pathological types of oropharyngeal cancer may be:
Squamous Cell Carcinoma: The most common type of oropharynx cancer is often called squamous cell carcinoma. These tumors arise from cells lining the surface of the oropharynx and can be divided into several subtypes.
Lymphoma: Types of cancer called lymphoma may also develop in the oropharynx area. These tumors arise from lymph tissue and differ from other types of oropharynx cancer.
Adenocarcinoma: Adenocarcinoma, a rare type, arises from the salivary glands or gland cells.
Mucoepidermoid Carcinoma: These tumors show a mixture of mucus-producing cells and epidermal cells.
Adenoid Cystic Carcinoma: A rarer type of cancer called adenoid cystic carcinoma is found in the oropharynx. These tumors usually grow slowly, but they can be aggressive.
The pathological type of oropharyngeal cancer may affect treatment options and prognosis. The treatment plan and prognosis are determined depending on the type of cancer, its stage, degree of spread, and the patient's health condition. Pathological examination helps create the correct diagnosis and treatment plan.There are some receptors and markers that should be examined in the treatment of oropharynx cancer. It is important to monitor these markers, especially in cases of HPV (Human Papillomavirus)-related oropharynx cancer. PD-1 (Programmed Death-1) and PD-L1 (Programmed Death Ligand-1) receptors used for immunotherapy treatment are important factors that regulate the patient's immune system attacking cancer cells. These markers are used to evaluate the patient's treatment response and personalize the treatment plan. However, each patient may be different, so receptor tests and markers should be determined by the doctor based on the patient's specific condition.
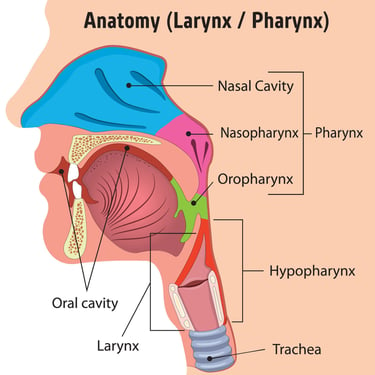
Image 2: Oropharynx cancer is a type of cancer that develops in the back of the oral cavity, in the pharynx (oropharynx) region.
HOW IS TUMOR STAGING DONE
Staging of oropharynx cancer is a system used to determine the extent and size of the cancer and its spread to the lymph nodes. This staging helps determine the patient's treatment plan and predict the prognosis of the disease. Staging of oropharynx cancer is usually done using the TNM system (Tumor, Node, Metastasis) or AJCC (American Joint Committee on Cancer) staging systems.
The basic components of these staging systems are:
T (Tumor Size): This part evaluates the size and location of the cancer. T stage is classified into grades ranging from T0 (no tumor) to T4 (tumor is large or has spread to surrounding tissues). The T1, T2, T3 and T4 subsections provide more detailed information based on the size and location of the tumor.
N (Lymph Nodes): This section evaluates the spread of the cancer to surrounding lymph nodes. N stage is classified into varying degrees from N0 (no lymph node involvement) to N3 (spread to surrounding lymph nodes).
M (Metastasis): This part evaluates whether the cancer has spread to other parts of the body. M stage is classified into varying degrees from M0 (no distant metastasis) to M1 (distant metastasis present).
These three components (T, N, and M) are used to determine the stage of the cancer. For example, T2N1M0 indicates that the tumor is of a certain size, has spread to a nearby lymph node, but has no distant metastasis.
Once the stage of the cancer is determined, the patient's treatment plan and prognosis are better understood. Staging helps determine how far the cancer has progressed and treatment options. Staging results are of great importance when creating a personalized treatment plan for each patient.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Treatment for oropharynx cancer may vary depending on the stage and type of cancer, the patient's general health status and other factors. Treatment according to stages is generally as follows:
Stage I and II:
Surgery: Surgery (for example, tonsillectomy) may be performed to remove small tumors.
Radiotherapy: Radiation therapy may be given to kill or control cancer cells.
Stages III and IV:
Combined Treatment: It may usually involve a combination of surgery, radiotherapy and chemotherapy. This treatment method is used to control or completely remove cancer.
Radiotherapy: In advanced stages, radiotherapy may be used to shrink the cancer or relieve symptoms.
Chemotherapy: Chemotherapy may be used to control the spread of cancer or to shrink the tumor before radiotherapy or surgery.
Recurrent Oropharynx Cancer: When cancer recurs or metastasizes to another area, the treatment plan is re-evaluated. In this case, new treatment options such as immunotherapy or targeted therapies may also be considered.
The treatment plan is determined depending on the individual situation of the patient and the characteristics of the cancer. New and developing treatment methods such as immunotherapy can also be used in some patients. During treatment, side effects and complications are also taken into consideration and the patient is closely monitored. Treatment of oropharynx cancer requires a multidisciplinary approach and collaboration between specialists such as an ear-nose-throat specialist, oncologist, radiation oncologist and surgeon.
Image 3: Oropharynx cancer can spread to the lymph nodes and cause swelling in the neck.
WHAT ARE THE SYSTEMIC DRUGS USED IN TREATMENT?
There are various drugs and treatment methods used in the treatment of oropharynx cancer. Here are some of these treatment options:
Chemotherapy: Platinum-Based Chemotherapy: Platinum-containing drugs, especially cisplatin and carboplatin, are frequently used in the treatment of oropharynx cancer. These drugs work by preventing the growth and proliferation of cancer cells.
EGFR (Epidermal Growth Factor Receptor) İnhibitörleri: EGFR inhibitors, such as cetuximab, may be used to treat some types of oropharyngeal cancer. EGFR is a protein that promotes the growth of cancer cells, so EGFR inhibitors work by blocking this function.
Immunotherapy: PD-1 or PD-L1 inhibitors, such as pembrolizumab and nivolumab, play an important role in the treatment of oropharynx cancer. These drugs encourage the immune system to attack cancer cells and may increase treatment response rates.
HPV Immunization Vaccine: To prevent cases of HPV-associated oropharyngeal cancer, HPV immunity vaccine (e.g., Gardasil 9) can be administered. The vaccine provides protection against HPV infections, especially at young ages.
Treatment options may vary depending on the patient's stage, type of cancer, and other personal factors. The treatment plan is determined by an oncologist or ear-nose-throat specialist based on the patient's specific condition. New treatment options are also being developed, so patients should have access to the most up-to-date information and treatment options.
HOW SHOULD FOLLOW-UP BE CARRIED OUT AFTER RECOVERY?
After oropharyngeal cancer treatment is completed, regular follow-up is necessary to monitor the patient's recovery progress and detect possible recurrences or complications. The follow-up plan is determined depending on the patient's response to treatment, the stage of the cancer, treatment methods and other factors. Follow-up usually includes the following elements:
Physical examination: Doctors regularly examine the patient's mouth, throat and neck area. It is examined carefully for any signs of tumor recurrence or symptoms.
Imaging Tests: Imaging tests such as computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) may be used to detect recurrence of cancer or new lymph node involvement.
Blood Tests: Blood tests can be used to evaluate levels of certain markers to monitor the return of cancer.
Smoking and Alcohol Counseling: Smoking and alcohol cessation programs and counseling services can be offered for patients who smoke or consume excessive alcohol.
Rehabilitation: Participation in rehabilitation programs may be encouraged to address post-treatment side effects that affect swallowing, speech, or other functions.
Follow-up periods may vary depending on the patient's response to treatment and risk factors. Post-recovery follow-up is vital for early detection of cancer and rapid response to treatment. Patients should keep regular follow-up appointments and report any symptoms or problems to their doctor immediately.