Oral Cavity Cancer
21.03.2024
ORAL CAVITY CANCER DIAGNOSIS AND TREATMENT


Oral cavity cancer is a type of cancer that occurs as a result of abnormal and uncontrolled growth of tissues in the oral cavity. The oral cavity includes the lips, tongue, gums, palate, pharynx, and intraoral mucosa. This type of cancer can occur for a variety of reasons, but the most common risk factors are associated with the use of tobacco products, excessive alcohol consumption, poor oral hygiene, and viral infections such as HPV (Human Papillomavirus) infection. Oral cavity cancer can lead to serious consequences if not diagnosed early. Therefore, it is important to pay attention to oral health, have regular dentist check-ups and minimize risk factors. Early diagnosis can increase the chances of treatment and improve quality of life. Additionally, avoiding risk factors such as smoking and alcohol can contribute to the prevention of oral cavity cancer. Therefore, protecting oral health and reducing risks is of great importance for the general health of the society
WHAT ARE THE RISK FACTORS?
There are a number of risk factors that increase the risk of developing oral cavity cancer. These factors may include:
Tobacco Use: Smoking, using cigars or pipes, and chewing tobacco products significantly increase the risk of oral cavity cancer. Chemicals in tobacco products can damage oral tissues.
Excessive Alcohol Consumption: Excessive alcohol consumption may increase the risk of oral cancer. Alcohol consumption along with tobacco use may further increase the risk.
Lack of Good Eating Habits: Inadequate fruit and vegetable consumption may increase the risk of oral cancer. These foods are rich in vitamins, minerals and antioxidants and are important in maintaining oral health.
HPV (Human Papillomavirus) Infection: Some high-risk types of HPV are viruses that can cause oral cavity cancer. This virus, which can be transmitted sexually, is a risk factor especially for mouth and pharynx cancers.
Familial History: The risk may increase in individuals with a family history of oral cavity cancer, which indicates that genetic factors may have an impact.
Gender: Men have a higher risk of developing oral cavity cancer than women.
Age: Oral cavity cancer is generally more common after the age of 40. The risk may increase with age.
Oral Hygiene: Not practicing regular oral hygiene and not paying attention to dental care can increase the risk of oral cavity cancer.
Intraoral Lesions: Oral sores, lesions or chronic irritations may increase the risk of cancer in the long term.
Sun Exposure: Types of cancer seen in the lower part of the lip or on the lips may be associated with long-term sun exposure.
You can reduce the risk of oral cavity cancer by taking these risk factors into account, making healthy lifestyle choices, and taking precautions such as regular dental check-ups. It is also important to contact a physician immediately when you see intraoral lesions or suspicious symptoms, because early diagnosis can be a great advantage in the fight against cancer.
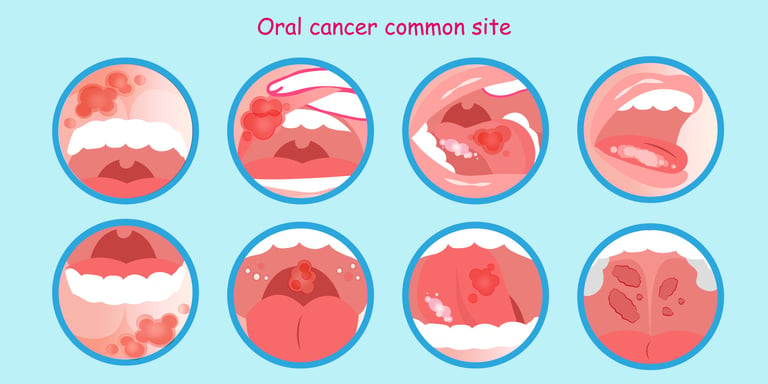
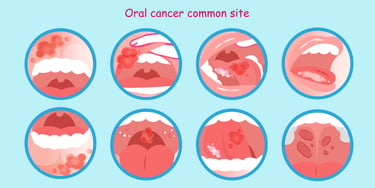
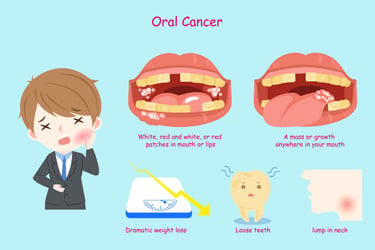
Image 1: Oral cavity cancer can occur in different areas within the mouth.
HOW DOES IT OCCUR?
The development mechanisms of oral cavity cancer involve a complex process. Generally, cancer cells begin when normal oral cells begin to grow abnormally as a result of genetic mutations. These mutations can be triggered by many different reasons, such as DNA damage, genetic factors, environmental factors (for example, tobacco products or alcohol use), or viral infections (for example, HPV). As a result of genetic changes, cancer cells multiply rapidly, replace normal cells and form tumors. Cancer cells can also spread (metastasize) to other parts of the body through blood or lymph. Factors that increase the risk of oral cavity cancer make these genetic changes more likely. Therefore, reducing risk factors and ensuring early diagnosis through regular health checks are important as preventive measures against the development mechanisms of oral cavity cancer.
WHAT ARE THE SYMPTOMS?
Oral cavity cancer is a type of cancer that occurs as a result of abnormal growth of tissues inside the mouth. Signs and symptoms of this cancer may include:
Intraoral Lesions: One of the most common symptoms of oral cavity cancer is the formation of lesions or sores inside the mouth. It can be alarming if these wounds do not heal for a long time or reappear.
Pain or Discomfort: Pain, soreness or discomfort in the mouth is a common symptom. There may be increased pain, especially during eating or speaking.
Tongue, Lip or Palate Changes: Oral cavity cancer can cause the lips, palate, or tongue to swell, change color, or change shape.
Sound Changes: Changes in voice quality may indicate types of cancer affecting the pharynx. In particular, hoarseness or a feeling of stuckness in the throat may be observed.
Intraoral Bleeding: Bleeding in the gums or inside the mouth may occur due to oral cavity cancer. Bleeding areas may be related to areas where there are wounds or lesions.
Swallowing Problems: Difficulty swallowing or painful swallowing is one of the symptoms of oral cavity cancer affecting the pharynx.
Weight Loss: Weight loss may occur due to factors such as loss of appetite, mouth pain and difficulty swallowing.
Earache: In some cases, oral cavity cancer may be associated with ear pain or ear discomfort.
An important point to note is that these symptoms alone do not always mean oral cavity cancer. However, if you experience these symptoms or have any concerns, you should consult a physician or dentist. Early diagnosis can increase the chances of treatment and prevent complications.
HOW IS IT DIAGNOSED?
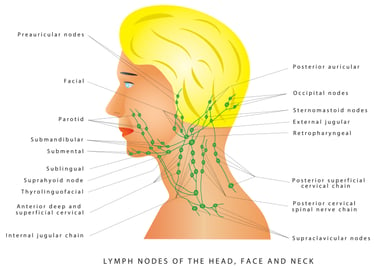
Oral cavity cancer is diagnosed using a number of clinical and laboratory methods. The first step is usually a physical examination and evaluation of the patient's symptoms. The doctor may examine oral lesions or abnormal tissues. Then, samples of suspicious tissue are taken in a process called biopsy and these samples are sent for laboratory tests. According to the biopsy results, cancer cells are detected and the type, stage and spread of the cancer are determined. Imaging methods, such as computed tomography (CT), magnetic resonance imaging (MRI), or positron emission tomography (PET), may be used to evaluate the extent of cancer spread. Lymph node biopsies may also be performed to see if it has spread to the lymph nodes. Diagnosis of oral cavity cancer is extremely important for early diagnosis and initiation of appropriate treatment. Therefore, it is important for people who show abnormal signs or symptoms inside the mouth to be evaluated by a physician as soon as possible.
WHAT ARE THE PATHOLOGICAL TYPES?
Oral cavity cancer can have different pathological types. These types are classified according to the morphological or histological characteristics of cancer cells and play an important role in treatment planning. Common pathological types of oral cavity cancer are:
Squamous Cell Carcinoma: Squamous cell carcinoma is the most common type of oral cavity cancer. In this type of cancer, flat, surface cells called squamous cells grow and divide abnormally.
Adenocarcinoma: Adenocarcinoma originates from tubular glands inside the mouth and is another common type of oral cavity cancer. This tumor originating from gland cells can be found especially in the salivary glands.
Adenosquamous Carcinoma: Adenosquamous carcinoma is a type of mixed tumor that has both glandular and squamous cell components.
Undifferentiated Carcinoma: In this type of cancer, it can be observed that the cells are not clearly differentiated and do not show typical features. This type of cancer can be aggressive and less likely to respond to treatment.
Oral cavity cancer may affect treatment approach and prognosis depending on its pathological type. Receptors to consider in oral cavity cancer treatment are proteins that control the growth and spread of cancer cells. Identification of these receptors allows the development of personalized treatment strategies. For example, therapies directed at targets such as EGFR, HER2, VEGFR, and immune-regulating receptors (PD-L1) may improve treatment responses of oral cavity cancer patients. Therefore, creating appropriate treatment plans according to the characteristics of the tumor, its stage and receptor expression can help patients achieve better results and increase the success in the fight against cancer. By focusing on these molecular targets, an important step is taken to develop more effective and less side-effect treatment options.
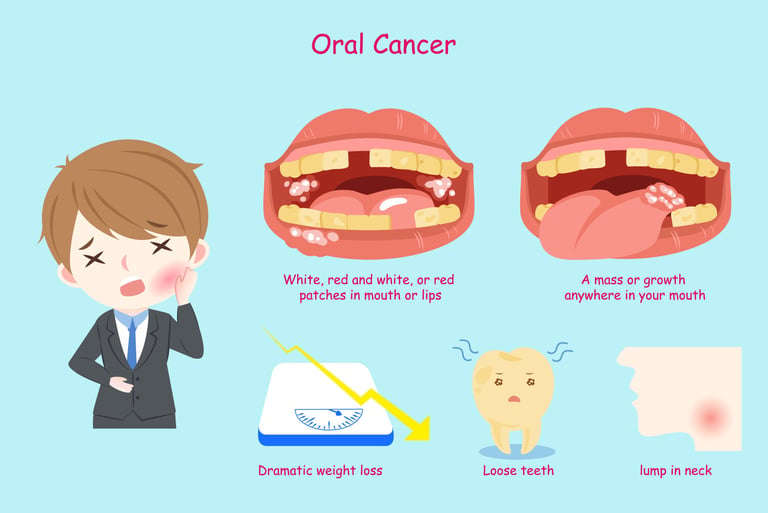
Image 2: Oral cavity cancer may cause complaints such as weight loss, tooth loss and neck swelling.
HOW IS TUMOR STAGING DONE?
Staging of oral cavity cancer is a method used to determine the extent, size and extent of spread of the cancer. This staging process is important when creating the treatment plan and assessing the patient's prognosis. Staging of oral cavity cancer is usually done by the following methods:
Physical examination: The doctor examines lesions, tumors and lymph nodes in the mouth, neck and surrounding areas. The size, location and other physical characteristics of the tumor are observed.
Imaging Tests: Imaging methods such as computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) are used to evaluate the size of the tumor, its extent of spread, and surrounding tissues.
Biopsy: The nature and pathology of the tumor is determined by a biopsy procedure. In this process, a tissue sample is taken from the tumor and sent for laboratory examination. Biopsy results help determine the pathological type and aggressiveness of the cancer.
Lymph Nodes: Oral cavity cancer often metastasizes to neck lymph nodes. Therefore, neck lymph nodes are also evaluated and, if necessary, a lymph node biopsy is performed.
Oral cavity cancer staging is generally based on the TNM classification system:
T (Tumor): It determines the size and extent of spread of the tumor.
N (Lymph Nodes): Evaluates the involvement of lymph nodes.
M (Metastasis): Determines whether there is metastasis to distant organs.
By bringing this information together, the stage of the cancer is determined. The staging process classifies the stage of cancer as follows:
Stage 0: Cancer is only superficial and locally limited.
Stage I: The tumor is small and locally limited.
Stage II: The tumor is larger and/or has spread to nearby lymph nodes.
Stage III: The tumor has grown larger and/or affected more lymph nodes.
Stage IV: Cancer has spread to peripheral tissues or distant organs.
This staging system plays an important role in determining treatment options and predicting the patient's prognosis. The treatment plan is personalized based on the patient's cancer stage, tumor size, and degree of spread.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Treatment for oral cavity cancer is individualized depending on the stage of the cancer, the size of the tumor, the extent of spread, and the patient's general health condition. Treatment may often involve different modalities such as surgery, radiotherapy, chemotherapy, or a combination of these.
Common treatment approaches according to oral cavity cancer stages:
Stage 0 and Stage I: In these early stages, tumors can often be removed surgically. Small tumors can be removed by local excision or minimally invasive surgery. Adjuvant treatment options such as radiotherapy or radiotherapy and chemotherapy may also be considered after surgery.
Stage II and Stage III: In these stages, tumors are larger and tend to spread to the lymph nodes. Treatment usually involves a combination of surgery, radiotherapy and/or chemotherapy. Surgery may include removing the tumor and cleaning the lymph nodes. Radiotherapy can be used after surgery or independently. It can be used in combination with chemotherapy, radiotherapy or after surgery.
Stage IV: In these stages, cancer is usually found at a more advanced stage and can spread to surrounding tissues or distant organs. Treatment may include a combination of surgery, radiotherapy and/or chemotherapy. Surgery may aim to remove the tumor or relieve symptoms. Radiotherapy and chemotherapy are used to shrink or control the tumor. At this stage, supportive care is also important in order to improve the quality of life of patients and relieve symptoms.
Each patient is different, and the treatment plan should be determined by his or her specific situation and the characteristics of the cancer. Your treatment team (surgeon, radiation oncologist, medical oncologist, dentist, etc.) will help you determine the most appropriate treatment approach. Supportive care is important to improve the patient's quality of life and reduce side effects during treatment. Therefore, patients and their families should communicate with their doctors to understand the treatment plan and results.
Image 3: Oral cavity cancers can spread to the lymph nodes in the neck and cause swelling.
WHAT ARE THE DRUGS USED IN TREATMENT
Some chemotherapies, hormonal drugs, smart drug treatments and immunotherapies used to treat oral cavity cancer include:
Chemotherapy drugs: Cisplatin, 5-Fluorouracil (5-FU), Docetaksel, Paklitaksel, Metotreksat, Bleomisin, Carboplatin
Smart Drug Therapies: Cetuximab (an EGFR inhibitor), afatinib
Immunotherapies: Pembrolizumab, Nivolumab
The treatment plan is determined depending on the patient's cancer type, stage and general health condition. Which medications to use and how the treatment will be administered are evaluated and individualized by an oncologist. Immunotherapies have begun to play an important role in the treatment of oral cavity cancer in recent years and may help the immune system target cancer cells. However, each treatment option has different side effects and benefits, and doctors perform medical evaluations to determine the best treatment for patients' conditions.
HOW SHOULD FOLLOW-UP BE DONE AFTER RECOVERY?
It is important that patients are included in a regular follow-up program after oral cavity cancer treatment is completed. This follow-up is done to detect early cancer recurrence, manage post-treatment side effects, and monitor the patient's general health. The follow-up program usually includes: regular doctor's exams, imaging tests (for example, CT or MRI), blood tests, and other appropriate medical tests. Patients are also encouraged to pay attention to oral hygiene, avoid smoking and alcohol consumption, and adopt a healthy lifestyle. Follow-up can improve patients' long-term health and quality of life by detecting cancer recurrence early and increasing the chances of starting treatment earlier. Therefore, it is important for them to follow a regular follow-up plan after cancer treatment.