Non-Hodgin Lymphoma
21.03.2025
DIAGNOSIS AND TREATMENT OF NON-HODGKIN LYMPHOMA
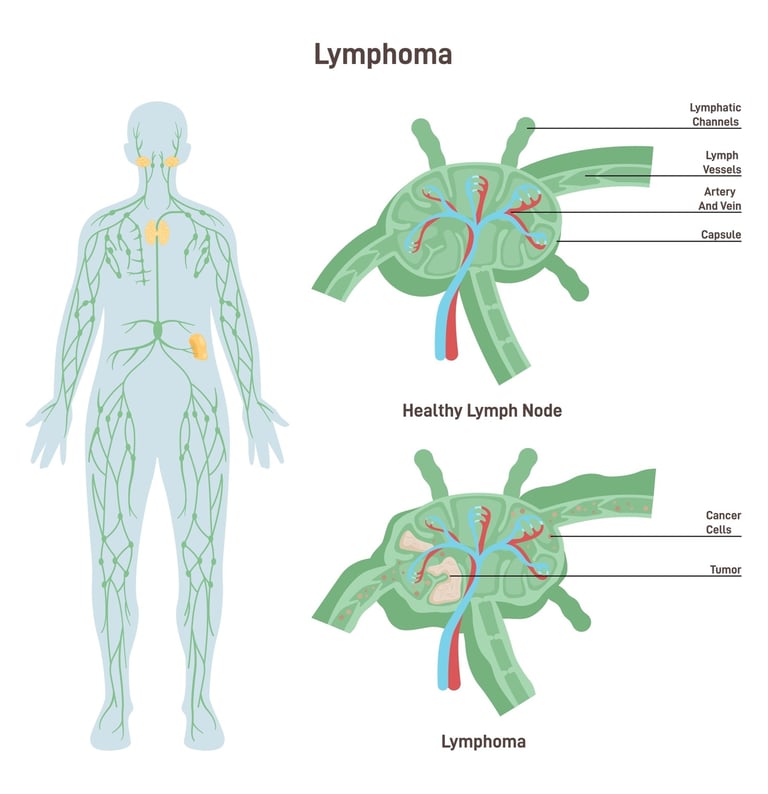
Non-Hodgkin Lymphoma (NHL) refers to a number of different types of cancer of the lymphatic system and includes diseases that affect the lymph nodes, spleen and immune system. Unlike Hodgkin Lymphoma, NHL involves a much more diverse range of cell types and subtypes and generally presents a more heterogeneous disease picture. The importance of NHL is increasing due to both its prevalence and diversity. Treatment methods and prognosis vary greatly depending on the specific subtype of NHL, the stage of the disease, and the patient's overall health. While some types of NHL may progress slowly and require minimal treatment, others may be much more aggressive and require intense chemotherapy or immunotherapy. Early diagnosis of NHL and access to appropriate treatment are important in managing the disease and improving patients' quality of life.
WHAT ARE THE RISK FACTORS?
Risk factors for Non-Hodgkin Lymphoma (NHL) include a variety of conditions that can contribute to the development of the disease. However, each of these factors does not mean that the disease will definitely develop. Some known risk factors for NHL:
Age: The risk of NHL increases with age. In most cases, it is more common in people over the age of 60.
Gender: Men have a slightly higher risk of developing NHL than women.
Immune System Weakness: Diseases that suppress the immune system, such as HIV/AIDS, or immunosuppressive drugs used after organ transplantation, may increase the risk of NHL.
Autoimmune Diseases: People with autoimmune diseases such as rheumatoid arthritis and Sjögren's syndrome have a higher risk of developing NHL.
Infections: Some infections, such as Helicobacter pylori, Hepatitis C virus, Epstein-Barr virus, and Human T-lymphotropic virus, may increase the risk of NHL.
Environmental and Occupational Exposures: Exposure to chemicals such as agricultural chemicals, pesticides, solvents, and some dyes may increase the risk of NHL.
Family History: NHL occurs more frequently in some families, but in the majority of cases a genetic link has not been clearly identified.
Radiation and Chemotherapy Exposure: The risk of NHL may be slightly increased in people who have had radiation therapy or chemotherapy in the past.
These risk factors may contribute to the development of Non-Hodgkin's Lymphoma, but the exact causes of the disease are still not fully understood. Most people do not develop NHL despite having one or more of these risk factors. On the other hand, people without any known risk factors can also develop this disease. Therefore, if there are symptoms or concerns, it is important to consult a healthcare professional.
Image 1: There are two main types of non-Hodgkin lymphoma, B-cell and T-cell, and many subtypes.
HOW DOES IT OCCUR?
The developmental mechanisms of Non-Hodgkin Lymphoma (NHL) are based on complex interactions of genetic and environmental factors, and there are many subtypes of this disease. The basis of NHL is uncontrolled cell growth and division in white blood cells known as lymphocytes. The formation of these abnormal cells is triggered by disruption of the normal function of regulatory genes as a result of mutations in the DNA. These genetic changes can activate pathways that prevent the death of cells (suppress apoptosis) and promote abnormal cell proliferation. Additionally, weakened immune systems, chronic inflammation, and certain virus infections (e.g., Epstein-Barr virus, Hepatitis C virus) may also play a role in the development of NHL. Environmental factors, chemical exposures, and some lifestyle factors may also increase the risk of NHL. However, the exact interplay and importance of these factors in each case of NHL varies greatly, and the heterogeneous nature of the disease makes it difficult to understand and treat. This complexity increases the importance of personalized approaches in the treatment and management strategies of NHL.
WHAT ARE THE SYMPTOMS?
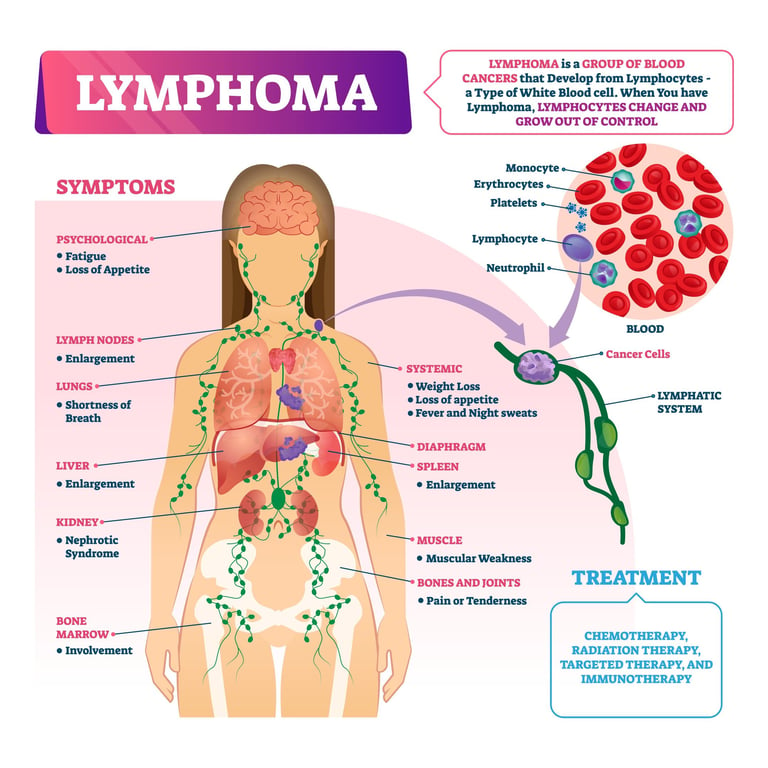
Because Non-Hodgkin Lymphoma (NHL) has several subtypes, its signs and symptoms can vary widely. However, the most common signs and symptoms are:
Lymph Node Swelling: Painless lymph node swelling in the neck, armpit or groin area is among the most common symptoms.
Fever and Night Sweats: Unexplained fever and intense sweating, especially at night, may occur.
Weight Loss: Unexplained and sudden weight loss may be a typical symptom of NHL.
Fatigue and Weakness: A constant feeling of fatigue and general weakness are common symptoms of lymphoma.
Loss of Appetite and Abdominal Pain: Pain or discomfort in the abdominal area and loss of appetite may occur due to enlargement of the spleen and/or liver.
Respiratory Problems and Cough: Respiratory problems such as cough, shortness of breath or chest pain may occur due to the enlargement of lymph nodes in the chest area.
Changes in the Skin: Some subtypes of NHL may cause changes in the skin, such as a rash or rash.
Immune System Weakness: Frequent infections and increased susceptibility to diseases may be an indication of a weakened immune system.
Since these symptoms can be seen in many different conditions other than NHL, medical evaluation and necessary tests must be performed for diagnosis. If you are experiencing any of these symptoms, it is important to consult a hematology or oncology doctor.
HOW IS IT DIAGNOSED?
The diagnosis of Non-Hodgkin Lymphoma (NHL) is made based on a comprehensive evaluation of the patient's symptoms, medical history, and a series of diagnostic tests. The diagnostic process usually begins with a physical examination of the patient; Here, the doctor checks for symptoms such as swelling of the lymph nodes and enlargement of the liver and spleen. The most critical step to confirm the diagnosis is the pathological examination of a biopsy sample taken from the affected lymph node or other tissues. Biopsy includes cell type, morphology, and in some cases molecular and genetic testing to determine the specific subtype of NHL. Additionally, blood tests, computed tomography (CT) scans, positron emission tomography (PET) scans, and sometimes bone marrow biopsy may be performed to evaluate the spread of disease throughout the body. These tests help determine the stage of the disease and create the most appropriate treatment plan. Non-Hodgkin Lymphoma is diagnosed through a comprehensive combination of these tests and evaluations and should always be conducted by an experienced hematology or oncology doctor.
WHAT ARE THE PATHOLOGICAL TYPES?
Non-Hodgkin Lymphoma (NHL) represents a broad group of cancers divided into many different pathological subtypes. These subtypes of NHL are classified based on the type of cells affected and the growth rate of the cancer. Here are the most common Non-Hodgkin Lymphoma subtypes:
B-Cell Lymphomas:
Diffuse Large B-Cell Lymphoma: The most common form of NHL and is a fast-growing, aggressive type of cancer.
Follicular Lymphoma: It is generally a slower-growing, indolent (low-grade) type.
Mantle Cell Lymphoma: It is a moderately fast-growing and more aggressive type of cancer.
Small Lymphocytic Lymphoma (SLL): It is a type of lymphoma that usually progresses slowly.
Burkitt Lymphoma: It is a very fast-growing and highly aggressive type of lymphoma.
T-Cell Lymphomas:
Peripheral T-Cell Lymphoma (PTCL): An often fast-growing type of lymphoma that has several different subtypes.
Anaplastic Large Cell Lymphoma (ALCL): Usually seen in young adults and children, it is a fast-growing type.
Cutaneous T-Cell Lymphoma (CTCL): A type of lymphoma that begins in the skin and usually progresses slowly.
Other Lymphomas:
Lymphoplasmacytic Lymphoma: It is a type of B-cell lymphoma and is usually a slow-growing cancer.
Marginal Zone Lymphoma: It is a slow-growing type of lymphoma that usually affects mucosal tissues.
These pathological subtypes are determined by the microscopic appearance, genetic characteristics, and clinical behavior of lymphoma cells. Diagnosis and treatment planning are based on detailed analysis of these subtypes, as each subtype may require different treatment approaches. Therefore, when NHL is diagnosed, it is vital to accurately determine the specific subtype and make an appropriate treatment plan. In the diagnosis and treatment of Non-Hodgkin Lymphoma (NHL), it is important to determine certain receptors and molecular markers according to the subtype and characteristics of the disease. These receptors and markers play critical roles in accurately classifying the disease, determining prognosis, and identifying potential treatment targets. Some receptors and markers often looked at in NHL include:CD20 (an especially important target in B-cell lymphomas),CD3 vs CD5 (Used in the diagnosis of T-cell lymphomas),CD10, BCL-2 ve BCL-6 (may have prognostic significance in some B-cell lymphomas), and Ki-67 (shows cell proliferation and can provide information about the aggressiveness of the disease). Additionally, in some subtypes of NHL, such as MALT lymphomas,Helicobacter pylori The presence of infection can also be investigated. These receptors and molecular markers are carefully studied by pathologists and oncologists and play an important role in determining the course of the disease as well as treatment options. Because each patient's situation is unique, the results of these tests should be evaluated individually and treatment approaches personalized.
Image 2: Lymphoma can cause fatigue, swelling in the lymph nodes, fever, and complaints depending on the organ it affects.
HOW IS TUMOR STAGING DONE?
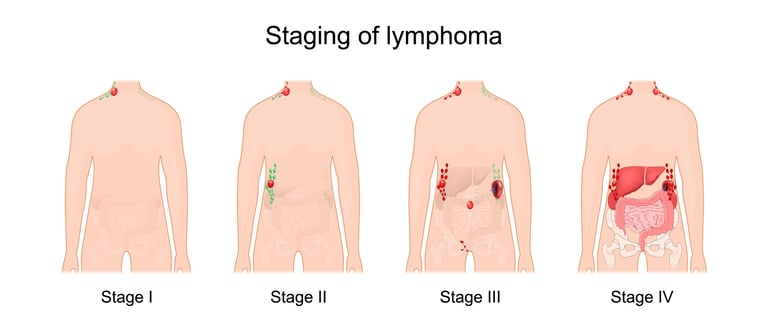
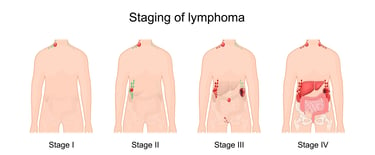
Tumor staging for Non-Hodgkin Lymphoma (NHL) is performed to determine how far the disease has spread in the body and is critical for treatment planning. Staging of NHL is usually done using the Ann Arbor Staging System, which is also used for Hodgkin Lymphoma. Here's the NHL's staging:
Stage I: Lymphoma is confined to a single lymph node area (I) or a single extra-lymphatic organ or area (IE) of the body.
Stage II: Lymphoma has spread to two or more lymph node regions, but these lymph nodes are on the same side of the diaphragm (II). This may also have spread to one or more extra-lymphatic organs or regions and lymph node areas (IIE).
Stage III: The lymphoma has spread to the lymph node areas on both sides of the diaphragm. This may also have spread to extra-lymphatic organs or sites (IIIE), the spleen (IIIS), or both (IIIES).
Stage IV: Lymphoma has spread to one or more extra-lymphatic organs or tissues, especially distant sites such as the bone marrow, liver, or brain.
Additionally, the letters "A" or "B" are used in the staging of NHL:
"A": There are no specific systemic symptoms such as fever, night sweats, or significant weight loss.
"B": The patient has certain systemic symptoms, such as fever, night sweats, or loss of more than 10% of body weight in the last six months.
Staging is based on the results of diagnostic tests, such as a physical examination, blood tests, lymph node biopsy, and imaging studies (PET scan, CT scan, etc.). This staging plays an important role in determining treatment options for the disease and assessing the patient's overall prognosis. The staging process should be performed by an experienced hematologist or oncologist.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
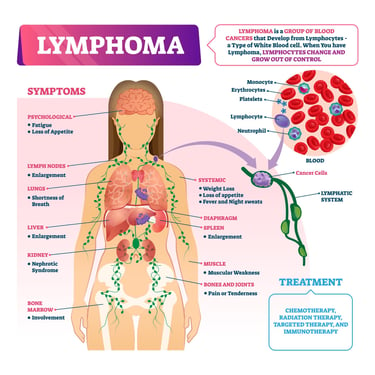
Treatment for Non-Hodgkin Lymphoma (NHL) is determined by the stage of the disease, its subtype, the patient's general health status, and other factors.
General treatment approaches according to the stages of NHL:
Stage I and II (Early Stage): Early-stage NHL usually requires localized treatment. This may include radiotherapy or combination chemotherapy directed to the affected area. Commonly used chemotherapy regimens for B-cell lymphomas include R-CHOP (rituximab, cyclophosphamide, hydroxydaunorubicin, oncovin, and prednisone) and similar combinations. Different chemotherapy regimens may be preferred for T-cell lymphomas.
Stages III and IV (Advanced Stage): Advanced-stage NHL usually requires more aggressive treatment. These treatments may include broad chemotherapy regimens and biological treatments (such as monoclonal antibodies). In advanced stages, treatment usually aims to control the disease and achieve remission. High-dose chemotherapy and autologous stem cell transplantation are also applicable treatment options in some cases.
Relapsed or Refractory (Treatment-Resistant) NHL: In cases of relapsed or treatment-resistant NHL, different approaches than standard chemotherapy may be required. In this case, treatment options such as next-generation targeted therapies (e.g., lenalidomide, ibrutinib), immunotherapies (e.g., CAR T-cell therapy), and sometimes allogeneic stem cell transplantation may be considered.
In the treatment of NHL, monitoring the general health of patients, managing side effects and supportive care are important. Treatment should be customized for each patient and managed by experienced oncology and hematology specialists. The treatment plan is personalized according to the characteristics of the disease, the patient's preferences and lifestyle. Regular medical follow-up and evaluations during the treatment process are an important part of treatment success.
Image 3: Non-Hodgkin lymphoma treatment is based on the subtype and stage of the disease.
WHAT ARE THE DRUGS USED IN TREATMENT?
In the treatment of Non-Hodgkin Lymphoma (NHL), chemotherapies, targeted (smart) drugs, immunotherapies and in some cases hormonal drugs are used. Here are some of these treatment options:
Chemotherapy pills
CHOP (Cyclophosphamide, Hydroxydaunorubicin, Oncovin [Vincristine], Prednisone): It is one of the most commonly used chemotherapy regimens.
R-CHOP: It consists of the addition of rituximab to the CHOP regimen and is especially effective for B-cell lymphomas.
CVP (Cyclophosphamide, Vincristine, Prednisone): Used in lower grade lymphomas.
Bendamustine: Often given together with rituximab and is effective for some B-cell lymphomas.
EPOCH (Etoposide, Prednisone, Vincristine, Cyclophosphamide, Hydroxydaunorubicin): Used for more aggressive types of NHL.
Targeted (Smart) Drugs
Rituximab: is a monoclonal antibody directed against CD20-positive B-cell lymphomas.
Ibrutinib: Bruton tyrosine kinase inhibitor, used primarily for Mantle Cell Lymphoma and some other lymphomas.
Imatinib and Dasatinib: Used in Philadelphia chromosome positive lymphomas.
Bortezomib: Proteasome inhibitor, used primarily in Mantle Cell Lymphoma and some other types of lymphoma.
Immunotherapies
CAR T-cell therapy: It is used especially in treatment-resistant or recurrent lymphomas.
Checkpoint Inhibitors (e.g., Pembrolizumab, Nivolumab): Used to activate the immune system against cancer cells.
Supportive Treatments
G-CSF (Granulocyte Colony Stimulating Factor): Used to increase the number of white blood cells after chemotherapy.
Erythropoietin: It can be used in cases of chemotherapy-related anemia (decrease in red blood cells).
These treatments are personalized according to the characteristics of the disease, the patient's general health condition and response to treatment. Treatment options and combinations are constantly evolving and should always be implemented in accordance with the most current medical guidelines and research. It is important that patients are evaluated by experienced oncologists before any treatment plan is initiated
HOW SHOULD FOLLOW-UP BE CARRIED OUT AFTER RECOVERY?
After completion of Non-Hodgkin Lymphoma (NHL) treatment, long-term follow-up of patients is important. Post-recovery follow-up is critical to monitor the potential for disease relapse, manage long-term side effects of treatment, and support overall patient health. This follow-up usually includes regular physical exams, blood tests, and imaging tests (for example, PET/CT scans) when necessary. Patients are called for more frequent check-ups during the first few years after treatment, as the risk of recurrence is highest during this period. The frequency of follow-up may decrease over time, but depending on the patient's condition, long-term follow-up may be required. Additionally, the potential long-term effects of NHL and its treatment are taken into consideration, particularly issues such as heart and lung health, risk of secondary cancers, and bone density. Patients are also informed about healthy lifestyle changes and risk reduction strategies. Regular medical follow-up and counseling for patients recovering from NHL are vital to maintaining a healthy life and minimizing potential complications. This process should be determined according to the individual needs of each patient and should be managed by experienced hematology or oncology physicians.