Lung Cancer
21.03.2025
LUNG CANCER DIAGNOSIS AND TREATMENT
Lung cancer is a serious type of cancer that occurs in the lung tissues and can progress rapidly. It is one of the most common types of cancer worldwide and one of the leading causes of cancer-related diseases. Lung cancer, which is generally associated with smoking, can also occur in non-smokers, and in this case, environmental factors or genetic predisposition may often be effective. There are two main types of lung cancer: small cell (SCLC) and non-small cell (NSCLC) lung cancer. While NSCLC accounts for approximately 85% of all cases, SCLC has a more aggressive course. Early diagnosis can significantly increase the chances of success in lung cancer treatment, but unfortunately in most cases cancer is diagnosed in advanced stages. Therefore, regular screening is important for individuals with risk factors. Lung cancer is an area of intense medical research, and new treatment methods (targeted therapies, immunotherapies) and early diagnosis techniques are promising in this field. The importance of this type of cancer is great not only for sick individuals and their families, but also for general healthcare systems, due to its high incidence and often poor prognosis.
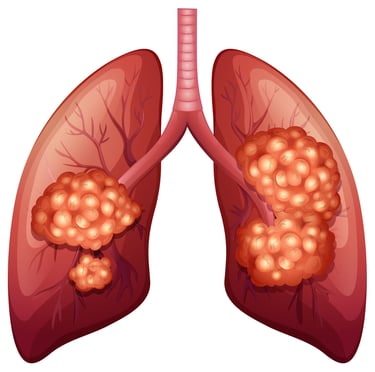
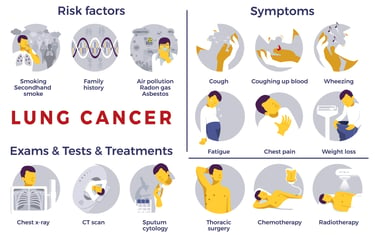
WHAT ARE THE RISK FACTORS?
Lung cancer can develop depending on various risk factors. Some of these factors can be modified (changed) and some cannot.
The most important risk factors of lung cancer:
Modifiable Risk Factors
Smoking:The majority of lung cancer cases are associated with active smoking. Exposure to second-hand smoke also increases the risk.
Radon Gas Exposure: Radon is a naturally occurring radioactive gas and may increase the risk of lung cancer when exposed to high levels.
Exposure to Asbestos and Other Carcinogenic Substances: Exposure to asbestos, arsenic, chromium, nickel, and some other industrial substances, especially in occupational environments, may increase the risk of lung cancer.
Air pollution: Long-term exposure to air pollution may increase the risk of lung cancer.
Lung Diseases: Previous lung diseases, such as chronic obstructive pulmonary disease (COPD) and fibrosis, may increase the risk of developing lung cancer.
Non-Modifiable Risk Factors
Age: The risk of lung cancer increases with age. Most cases of lung cancer are diagnosed in people aged 65 and over.
Gender: Men have a slightly higher risk of lung cancer than women, but this difference decreases with changes in smoking rates.
Family History of Lung Cancer: Individuals with a family history of lung cancer have a higher risk of developing this cancer.
Genetic predisposition: Some genetic mutations may increase the risk of developing lung cancer.
Some of these risk factors, especially smoking and exposure control, can be reduced by personal preferences and lifestyle changes. Early diagnosis and management of risk factors are among the important strategies in the fight against lung cancer.
Genetic risk factors and familial transmission in lung cancer are among the important factors in the development of this disease. Genetic factors can influence a person's susceptibility to lung cancer, but in most cases, cancer is more closely related to environmental factors and lifestyle choices. In addition to factors such as smoking and exposure to asbestos, some genetic mutations may also increase the risk of lung cancer. In particular, people with a family history of lung cancer have a higher susceptibility to cancer. Some types of lung cancer, particularly non-small cell lung cancer (NSCLC), may show a more distinct pattern of genetic predisposition. Genetic factors may be more prominent in certain subtypes of cancer, such as those susceptible to targeted treatment options, such as EGFR or ALK gene mutations. However, in general, lung cancer is not considered a disease with familial transmission, although there may be a genetic predisposition in individuals with more than one case in the family. Therefore, it is recommended that high-risk individuals receive genetic counseling and genetic testing when necessary. This is especially true for people with a family history or other risk factors. Such genetic counseling and testing can help an individual better understand their risk and identify early detection strategies.
Image 1: Smoking is responsible for 80-90% of all lung cancer cases in society.


HOW DOES IT OCCUR?
The development of lung cancer results from the disruption of the normal growth and division pattern of cells, and this process occurs through the interaction of a number of genetic and environmental factors. DNA damage in lung cells can lead to genetic mutations, resulting in uncontrolled proliferation of cells and tumor formation. Carcinogenic substances such as cigarette smoke are the main causes of these mutations by damaging DNA in lung cells. Damaged DNA can lead to activation of oncogenes (cancer-associated genes) or inactivation of tumor suppressor genes, resulting in abnormal behavior of cells and the development of cancer. Additionally, disruption of the self-destruction (apoptosis) mechanism of cells may also play a role in tumor development. Chronic inflammation and ongoing damage and repair processes in lung tissue may also contribute to the development of lung cancer. These complex interactions determine the various types of lung cancer and the course of the disease, and therefore treatment strategies must be determined taking this diversity and complexity into account.
WHAT ARE THE SYMPTOMS?
Lung cancer often has no symptoms in its early stages, making early diagnosis difficult. However, various symptoms may be observed in later stages. Common signs of lung cancer include:
Cough: A chronic, persistent cough that gets worse over time is one of the most common symptoms of lung cancer.
Shortness of breath: Shortness of breath may occur due to the tumor blocking the airways or affecting lung functions.
Chest Pain: Pain or discomfort in the chest, back or shoulders may occur, especially when breathing deeply or coughing.
Bloody Phlegm: Blood or bloody sputum may be detected when coughing.
Hoarseness: Hoarseness or changes in voice may occur as a result of the larynx being affected.
Difficulty Swallowing: It can be seen especially in tumors close to the esophagus.
Weight Loss and Loss of Appetite: Unexplained weight loss and loss of appetite may occur.
Fatigue and Weakness: There may be a general feeling of fatigue and lack of energy.
Frequent Infections and Fever: Frequent infections such as bronchitis or pneumonia and fever may be detected
Lymph Node Swelling: Swelling of lymph nodes in the neck or armpit may occur
These symptoms may also occur for conditions other than lung cancer, so it is important for individuals with such symptoms to consult a physician for a definitive diagnosis. Early diagnosis can significantly increase treatment success.
HOW IS IT DIAGNOSED?
Lung cancer is diagnosed through a series of medical tests and evaluation processes. First, the patient's symptoms, medical history, and risk factors are evaluated by the doctor. Imaging tests are then performed for suspicious symptoms; these may include a chest X-ray, computed tomography (CT) scan, and positron emission tomography (PET) scan. If these tests support the suspicion of cancer, a biopsy is performed to make a definitive diagnosis. During the biopsy process, a small sample of lung tissue is taken and examined under a microscope. Biopsy is used to determine the presence of cancer cells, the type of cancer, and the characteristics of the cancer cells. Additionally, additional procedures may be required in some cases, such as bronchoscopy. Genetic and molecular testing can be particularly helpful in determining targeted treatment options. This process allows lung cancer to be diagnosed accurately and an effective treatment plan to be created. Diagnosis is performed in collaboration with oncologists, radiologists, pathologists and other physicians.
WHAT ARE THE PATHOLOGICAL TYPES?
Lung cancer is generally classified into two main pathological types: Non-Small Cell Lung Cancer (NSCLC) and Small Cell Lung Cancer (SCLC).
Non-Small Cell Lung Cancer (NSCLC): This type, which accounts for approximately 75-80% of lung cancers, generally spreads more slowly. NSCLC is classified into four main groups:
Adenocarcinoma: It is the most common subtype of lung cancer and is usually seen in non-smoking and female patients.
Squamous Cell Cancer: It usually develops in the large airways of the bronchi and is often seen in smokers.
Large Cell Cancer: This type is defined as different from the other two types and usually has a more aggressive course.
Mixed Type Cancers: This group includes cancers that have characteristics of more than one type.
Small Cell Lung Cancer (SCLC): It accounts for approximately 15% of all lung cancers and occurs mostly in smokers. This type tends to grow and spread rapidly and is usually found in an advanced stage at the time of diagnosis.
Both main types are characterized by an uncontrolled proliferation of cells in the lung tissue, and treatment methods are determined by the type and characteristics of the cancer.
Image 2: There are also many genetic and environmental factors in the development of lung cancer.
WHAT DOES PATHOLOGY EXAMINATION COVER?
Receptors to consider in lung cancer treatment may vary depending on the type of cancer and the characteristics of the patient. However, in general, important receptors to be examined in lung cancer may be:
Epidermal Growth Factor Receptor (EGFR) Reseptörü: EGFR mutations are important in lung cancer treatment. EGFR inhibitors may be effective in patients with these mutations.
Anaplastic Lymphoma Kinase (ALK) Receptor: ALK gene changes can be found in some types of lung cancer. ALK inhibitors can be used in such patients.
ROS1 Receptor: Although ROS1 gene changes are rare, ROS1 inhibitors may be a treatment option for patients with such changes.
BRAF Receptor: BRAF gene mutations can be seen in some lung cancer patients. BRAF inhibitors can be used for these patients.
Programmed Death-Ligand 1 (PD-L1): PD-L1 positivity is important in choosing immunotherapy treatment. Patients with high PD-L1 positivity may respond to PD-1 or PD-L1 inhibitors.
Kirsten Rat Sarcoma (KRAS) Gen: KRAS mutations are found in a subset of lung cancer patients. Efforts are being made to develop special treatment options for these patients. There are smart drugs in use for the KRAS G12C mutation.
MET Receptor: MET gene changes may be important in lung cancer treatment and MET inhibitors may be used.
RET Receptor: Although RET gene changes are rare, RET inhibitors may be effective for patients with such changes.
These receptors and gene changes are examined depending on the patient's medical history and the type of cancer. The treatment plan is personalized based on the presence of these receptors and gene changes. Therefore, it is important to seek the advice of an oncologist when creating a specific treatment plan for each patient.
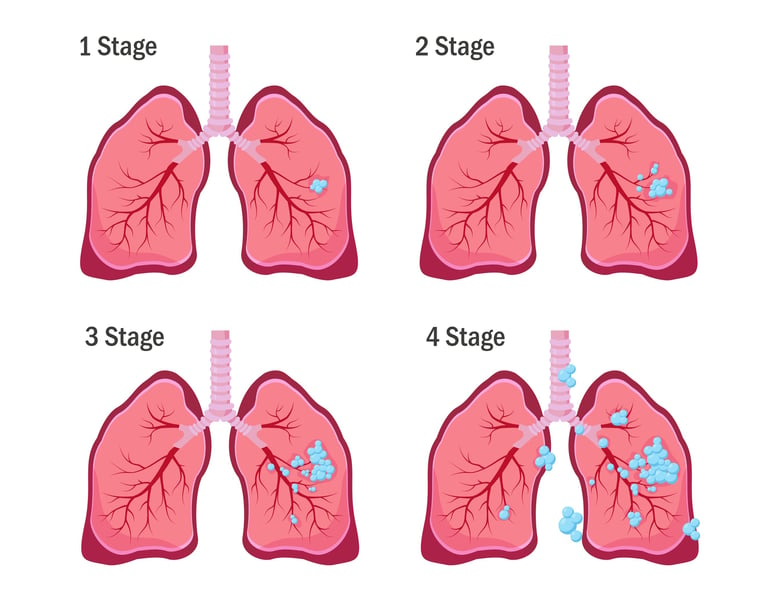
HOW IS STAGING DONE?
Staging is usually done using the "TNM" system:
T: Size and location of the tumor.
N: Lymph node involvement.
M: Presence or absence of distant metastasis.
Based on this information, cancer is classified into one of the following stages:
Stage 0: The cancer is only at the starting point and has not spread to lymph nodes or other organs.
Stage I: The cancer is confined to the lung and has not spread.
Stage II: Cancer may have grown in the lung and spread to some nearby lymph nodes.
Stage III: Cancer may have grown in the lung and spread to surrounding lymph nodes or nearby organs.
Stage IV: The cancer has metastasized (spread) to organs other than the lung.
Staging results play an important role in determining the patient's treatment options and prognosis. Therefore, accurate and complete staging is very important for patients diagnosed with lung cancer. Staging is done by an oncologist and helps determine the patient's treatment plan.
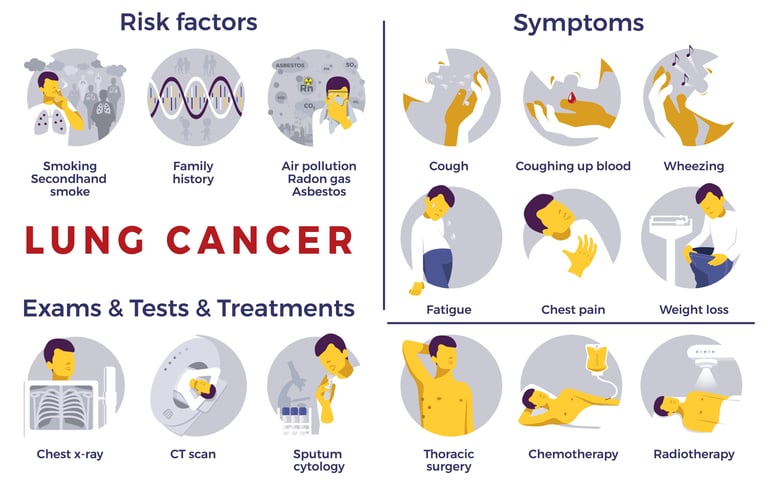
Image 3: Lung cancer treatment is performed according to the initial tumor stage.
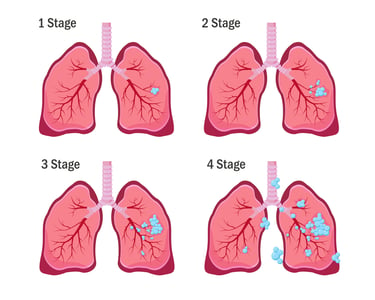
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Treatment options for lung cancer vary depending on the stage of the cancer. From a general perspective, treatment approaches according to these stages are as follows.
Early Stage Lung Cancer (Stage I and II):
Surgery: If the tumor is small enough and has not spread to other parts of the body, surgery to remove the entire tumor is the main treatment method.
Radiotherapy: May be used if surgery is not possible or as additional treatment.
Chemotherapy: May be used in some patients after surgery to prevent cancer from returning.
Locally Advanced Lung Cancer (Stage III):
Chemoradiotherapy: Chemotherapy and radiotherapy are often used together.
Surgery: In some cases, surgery may be possible, especially after the tumor has been reduced in size.
Targeted therapies and immunotherapy: May be used for tumors that carry certain genetic changes or to help the immune system fight cancer.
Metastatic Lung Cancer (Stage IV):
Targeted therapies: Drugs that target specific genetic mutations or proteins can be used.
Immunotherapy: Helps the immune system recognize and destroy cancer cells.
Chemotherapy: May be used to control the spread of cancer.
Palliative care: Focuses on relieving symptoms and improving quality of life.
Each patient's situation is unique and the treatment plan should be individually determined. Therefore, it is important to have a detailed evaluation with an oncologist to determine the most appropriate treatment methods. Lung cancer treatment is constantly evolving and new treatment options are under investigation.
WHAT ARE THE DRUGS USED IN TREATMENT?
There are various medications and treatment methods used in the treatment of lung cancer. These methods can be categorized as chemotherapies, hormonal drugs, targeted (smart) drug treatments and immunotherapies. Here are some examples of these types of treatments:
Chemotherapy Drugs:
Cisplatin
Karboplatin
Docetaxel
Paklitaxel
Gemcitabine
Vinorelbine
The pemetrexed
Targeted (Smart) Drug Therapies:
EGFR inhibitors (eg, Erlotinib, Gefitinib, Afatinib)
ALK inhibitors (e.g., Crizotinib, Ceritinib, Alectinib)
BRAF inhibitors (e.g., Dabrafenib, Vemurafenib)
ROS1 inhibitors (e.g., crizotinib)
MET inhibitors (e.g., Capmatinib, Tepotinib)
RET inhibitors A(e.g., Selpercatinib, Pralsetinib)
Immunotherapies:
PD-1/PD-L1 inhibitors (e.g., Pembrolizumab, Nivolumab, Atezolizumab)
CTLA-4 inhibitors (e.g. ipilimumab)
These drugs and treatment methods can be used in different ways and combinations depending on the type and stage of lung cancer, the patient's general health condition and the genetic characteristics of the cancer. Therefore, the treatment plan must be determined by the oncologist specifically for each patient. Additionally, new medications and treatments for lung cancer are constantly being developed, so it is important to consult with medical professionals for the most up-to-date information.
HOW TO FOLLOW UP AFTER RECOVERY?
Follow-up after recovery from lung cancer is vital for ongoing monitoring of the patient's health and early detection of cancer recurrence or other complications. This monitoring is usually accomplished through regular physical examinations, chest X-ray or computed tomography scans, and blood tests. The frequency of follow-up is generally more frequent in the first two years after treatment and may decrease over time. Patients are also trained for specific symptoms, such as new or worsening cough, shortness of breath, pain, or weight loss, that may require re-evaluation. The follow-up plan after lung cancer treatment is customized based on the type of cancer the patient initially had, the type of treatment, and his or her overall health. Additionally, patient support and rehabilitation programs can be important as part of the recovery process. During this process, smoking cessation and healthy lifestyle choices are also critical to improving the patient's overall health and reducing the risk of relapse.