Liver Cancer
21.03.2025
LIVER CANCER DIAGNOSIS AND TREATMENT
Liver cancer is a type of cancer caused by abnormal cells that multiply uncontrollably in liver cells. The liver, one of the largest organs in the human body, plays a critical role in the body's detoxification, metabolism and digestive processes. Therefore, liver cancer can cause serious health problems for the body. The most common types are hepatocellular carcinoma and cholangiocarcinoma. Risk factors include hepatitis B and C infections, chronic alcohol use, obesity and diabetes. Early diagnosis can significantly increase treatment options and the patient's survival rate. Therefore, it is of great importance for individuals with risk factors to have regular health checks and make lifestyle choices that protect liver health.
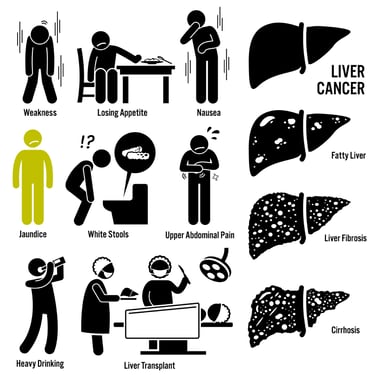
WHAT ARE THE RISK FACTORS?
Liver cancer risk factors include various factors that increase the likelihood of developing the disease. These factors include:
Hepatitis B and C Infections: Chronic hepatitis B or C infection significantly increases the risk of liver cancer.
Cirrhosis: Cirrhosis, a chronic disease of the liver, increases the risk of developing liver cancer.
Family History: Family members with liver cancer may increase the risk of developing the disease.
Alcohol Use: Excessive alcohol consumption can damage the liver over time, increasing the risk of cancer.
Obesity and Diabetes: Obesity and type 2 diabetes may increase the risk of liver cancer.
Exposure to Aflatoxins: Aflatoxins, produced by some molds and found especially in grains and peanuts, may increase the risk of liver cancer.
Iron Loading: Conditions such as hemochromatosis can cause iron accumulation in the liver and increase the risk of cancer.
Smoking: Smoking may also increase the risk of liver cancer.
Each of these factors can contribute to the development of liver cancer. However, the presence of these factors does not necessarily mean that it will lead to cancer. Each individual's risk varies depending on genetic, environmental and lifestyle factors. Preventive health measures and regular medical checkups can be important in reducing risk.
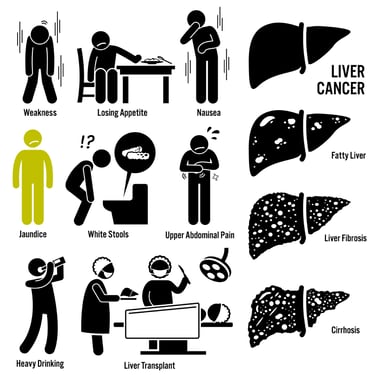
Image 1: Many complaints such as fatigue, weight loss and jaundice may be observed in liver cancer.
HOW DOES IT OCCUR?
The mechanisms of liver cancer development involve complex interactions of genetic and environmental factors. Cancer usually results from DNA damage in liver cells. This damage can lead to mutations in the genes that control cell division, disrupting normal cell growth and death processes, leading to uncontrolled cell proliferation and tumor formation. Chronic viral infections, such as hepatitis B and C, can lead to inflammation and eventually DNA damage in liver cells. Additionally, chronic liver diseases such as cirrhosis can cause constant renewal of cells and possible errors in this process. Exposure to toxins such as aflatoxin, alcohol consumption and obesity can also increase the risk of cancer by triggering DNA damage. The combination of these factors can lead to the accumulation of abnormal cells in the liver and ultimately cancer.
WHAT ARE THE SYMPTOMS?
Symptoms of liver cancer usually appear in the advanced stages of the disease. These symptoms may include:
Abdominal Pain and Bloating: Pain and discomfort, especially in the upper right part of the abdomen. Abdominal bloating may occur due to enlargement of the liver.
Jaundice:Yellowing of the skin and whites of the eyes as a result of the liver not being able to perform its functions.
Weight Loss and Loss of Appetite: Unexplained and significant weight loss and decreased appetite.
Fatigue and Weakness: A constant feeling of fatigue and weakness.
Nausea and Vomiting: Nausea and vomiting due to digestive problems.
Fever: Low-level fever can sometimes be associated with liver cancer.
Liver Enlargement: An enlarged liver that can be felt by the doctor on physical examination.
Abnormality in Liver Function Tests: Abnormal results in liver function tests.
These symptoms do not always mean liver cancer and may be related to other health problems. If you are experiencing such symptoms, it is important to consult a healthcare professional. Early diagnosis is an important factor in liver cancer treatment.
HOW IS IT DIAGNOSED?
The diagnosis of liver cancer is made using evaluation of clinical symptoms, laboratory tests and imaging methods. It usually begins with a medical history and physical examination of the patient. At this stage, blood tests such as liver function tests are performed, which provide information about the functioning of the liver and may indicate signs of cancer. Imaging tests such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI) are used to detect abnormalities and the presence of tumors in the liver. Based on imaging results, suspicious areas may be biopsied; Here, tissue samples are taken using a medical needle and examined under a microscope. The diagnosis of liver cancer is usually confirmed by biopsy because this method gives accurate results in determining whether the tumor is cancerous and the type of cancer. During the diagnosis process, the patient's general health condition and the degree of spread of the cancer are also evaluated.
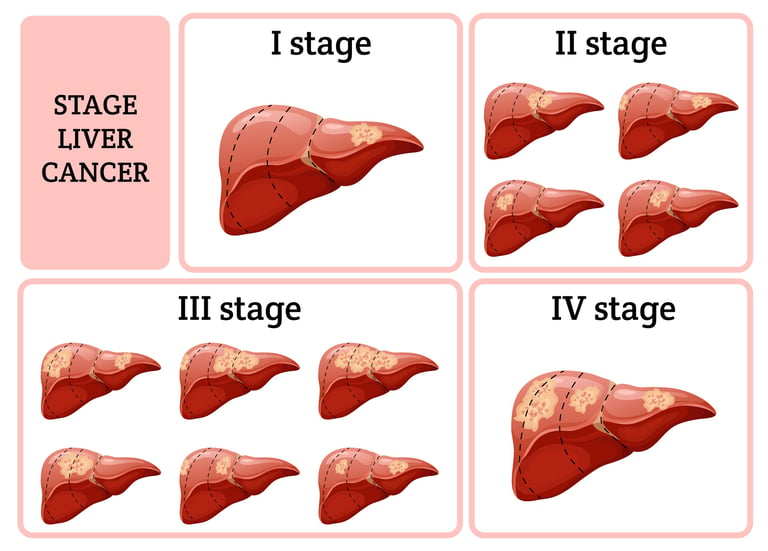
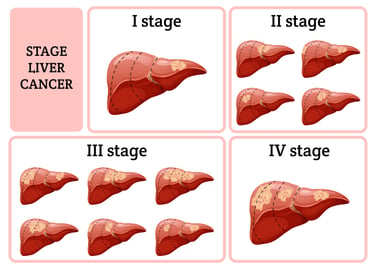
Image 2: Treatment selection for liver cancer is made according to the stage of the disease.
WHAT ARE THE PATHOLOGICAL TYPES?
There are various pathological types of liver cancer and they can arise from different types of cells in the liver. The most common types of liver cancer are:
Hepatocellular Carcinoma (HCC): This type, which accounts for the majority of liver cancers, arises from hepatocytes, the main cell type of the liver. Hepatocellular carcinoma is especially common in patients with chronic hepatitis and cirrhosis.
Cholangiocarcinoma (Bile Duct Cancer): It develops from the cells lining the inner surface of the bile ducts. It accounts for a small percentage of liver cancers and usually presents with symptoms such as blockage of the bile ducts.
Fibrolamellar HCC: This rare type of hepatocellular carcinoma is more common in young adults and generally has a better prognosis. Fibrolamellar HCC has microscopic features that differ from typical HCC.
Angiosarcoma and Hemangiosarcoma: These very rare types of cancer originate in the blood vessels of the liver.
Liver Metastases Cancer (Secondary Liver Cancer): Some cancers in the liver develop through metastases from primary tumors elsewhere in the body (for example, colon, breast, or lung cancer).
Each pathological type shows different clinical features and treatment responses. Therefore, it is important to determine the pathological type of cancer for accurate diagnosis and effective treatment planning. There are some receptors and molecular markers in liver cancer that are important in treatment planning and prognosis determination. Particularly in the case of hepatocellular carcinoma (HCC), various biological molecules present on or within the surface of cancer cells that may influence the behavior of the disease are examined. These include Epidermal Growth Factor Receptor (EGFR), Vascular Endothelial Growth Factor (VEGF) and its receptors, and Hepatocyte Growth Factor (HGF) and c-Met receptor. Some of these molecules may support the tumor to grow, metastasize, and form blood vessels. Additionally, immuno-oncological markers such as Programmed Cell Death Protein 1 (PD-1) and its ligand PD-L1 are also used to determine immunotherapy response. The presence and activity of these receptors are critical in determining the effectiveness of new treatment options, especially targeted therapies and immunotherapy. Therefore, when liver cancer is diagnosed, analysis of these receptors and markers plays an important role in personalizing the patient's treatment protocol.
HOW IS TUMOR STAGING DONE?
Tumor staging in liver cancer is a system used to determine the extent of spread and severity of cancer. This staging is based on factors such as the size of the cancer, its spread within the liver, and its spread to lymph nodes and other organs. The following steps are usually followed in the staging process:
Size and Number of Tumor (T): The size of the tumor and how many tumors there are in the liver are evaluated. This is used to determine the "T" category of the tumor.
Lymph Nodes (N): It is checked whether the cancer has spread to nearby lymph nodes. Involvement of lymph nodes determines the "N" category of cancer.
Metastasis (M):It is checked whether the cancer has spread outside the liver, especially to distant organs and tissues. This determines the "M" category.
Various imaging tests are used for this, such as ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), and sometimes positron emission tomography (PET) scans. Sometimes tissue samples taken during biopsy or surgery can also contribute to staging.
There are several different staging systems used for liver cancer. The most common of these are the TNM system used by the American Cancer Society and the Barcelona Clinic Liver Cancer (BCLC) staging system. BCLC also takes into account the patient's general health status and liver function, so it is often preferred in treatment planning. These staging processes are critical for planning treatment of liver cancer and assessing prognosis. The most appropriate treatment method (surgery, radiotherapy, chemotherapy, targeted therapy or immunotherapy) is determined according to the patient's stage.
HOW IS TREATMENT DONE ACCORDING TO TUMOR STAGES?
Treatment options for liver cancer are determined according to the stage of the disease and different treatment strategies can be applied for each stage:
Early Stage (Stage 0 and A): Tumors at this stage are usually small and limited. Surgical removal of the entire tumor (resection) or local treatments (such as radiofrequency ablation or microwave ablation) may be preferred to destroy the tumor. These treatments can stop or slow the progression of the disease.
Middle Stage (Stage B): At this stage, the tumor is either very large or there is more than one tumor, but the liver is functioning well and the cancer has not spread outside the liver. Localized treatments such as transarterial chemoembolization (TACE) are commonly used at this stage. TACE aims to stop the growth of the tumor by blocking the blood vessels feeding the tumor and applying chemotherapy drugs directly to the tumor.
Advanced Stage (Stage C): At this stage, the cancer has spread outside the liver or spread to the blood vessels. In this case, systemic treatments are preferred. Targeted therapies (such as sorafenib, lenvatinib) and immunotherapy (such as nivolumab, pembrolizumab) are used to slow the spread of cancer and improve the patient's quality of life.
Final Stage (Stage D): The cancer has spread severely and liver functions have deteriorated. The focus of treatment at this stage is on relieving symptoms and increasing the patient's comfort (palliative care). Pain control, nutritional support and other supportive treatments become important at this stage.
When determining treatment options according to the stage of liver cancer, factors such as the patient's general health condition, the status of liver functions and the characteristics of the cancer are also taken into consideration. Liver transplant may also be an option for some early-stage liver cancer patients. The most appropriate treatment plan for each patient is determined by oncologists, hepatologists, radiologists and other health professionals with a multidisciplinary approach.
Image 3: Surgery, RF, TACE and smart drug treatments can be applied in liver cancer.

WHAT ARE THE SYSTEMIC DRUGS USED IN TREATMENT?
Treatment methods used in liver cancer include chemotherapies, hormonal drugs, smart drug therapies (targeted therapies) and immunotherapies. Examples of each type of treatment include:
Chemotherapy Drugs:
Doxorubicin
Cisplatin
5-fluorouracil (5-FU)
Gemcitabine
Oxaliplatin
Smart Drug Therapies (Targeted Therapies):
Sorafenib: Used in the treatment of hepatocellular carcinoma (HCC) and inhibits the growth of tumor cells and the formation of new blood vessels.
Lenvatinib: It is another targeted therapy option used in the treatment of HCC.
Regorafenib: Used in advanced stages of HCC and may be an option for sorafenib-resistant cases.
Cabozantinib: It is also used in the treatment of HCC and is effective against tumor growth.
Immunotherapies:
Nivolumab: It is an immunotherapy drug belonging to the PD-1 inhibitor class and is used in some HCC patients.
Pembrolizumab: It is also a PD-1 inhibitor and is effective in the treatment of liver cancer.
Combination of Atezolizumab and Bevacizumab: The combination of PD-L1 inhibitor and VEGF inhibitor is used as a new approach in the treatment of HCC.
The use of these drugs varies depending on the stage of the cancer, the patient's general health condition and previous treatment responses. Treatment options should be evaluated individually for each patient by an oncologist. In cancer treatment, it is also important to manage the side effects of these medications and maximize the patient's quality of life.
HOW SHOULD FOLLOW-UP BE CARRIED OUT AFTER RECOVERY?
Follow-up after recovery from liver cancer is vital to detect early recurrence of the disease and monitor the patient's overall health. This process is often customized based on the patient's completed treatment and the unique characteristics of the cancer. Regular medical checkups are typically performed at 3 to 6 month intervals for the first few years. These checkups may include blood tests (liver function tests and tumor markers), imaging tests (such as ultrasound, CT, or MRI), and physical exams. Additionally, patients are encouraged to make lifestyle changes (eat a healthy diet, reduce alcohol consumption, exercise regularly) and continue management of conditions such as chronic hepatitis if present. It is important to see a doctor immediately with any new symptoms or concerns. The follow-up process may continue for years, depending on the type of cancer, its stage, and response to treatment. During this time, psychological and social support is also an important component to improve patients' quality of life during the recovery process.