Kidney Cancer
21.03.2025
KIDNEY CANCER DIAGNOSIS AND TREATMENT


Kidney cancer is a condition in which cells in the kidneys grow uncontrollably and form malignant tumors. Kidneys are the main organs that filter waste from the body, create urine, regulate blood pressure and produce various important hormones. Kidney cancer usually affects a single kidney, but in some cases, cancer can develop in both kidneys. The most common type is known as renal cell carcinoma (RCC) and begins in the tubules of the kidney. Another type is urothelial carcinoma, which can affect the parts of the kidney connected to the urinary tract. While kidney cancer does not cause symptoms at first, as it progresses, it may cause symptoms such as bloody urine, persistent back pain and weight loss. Early diagnosis is important for the success of treatment because the best treatment results can be achieved before the cancer spreads. Treatment methods include surgery, radiation therapy, chemotherapy, immunotherapy and targeted therapies. Kidney cancer is more common, especially in older men, but genetic factors and lifestyle choices (for example, smoking) may also increase the risk. The importance of this type of cancer is that it can affect the success of treatment, mainly due to the critical roles of the functionally important kidneys and its tendency to show no symptoms in the early stages.
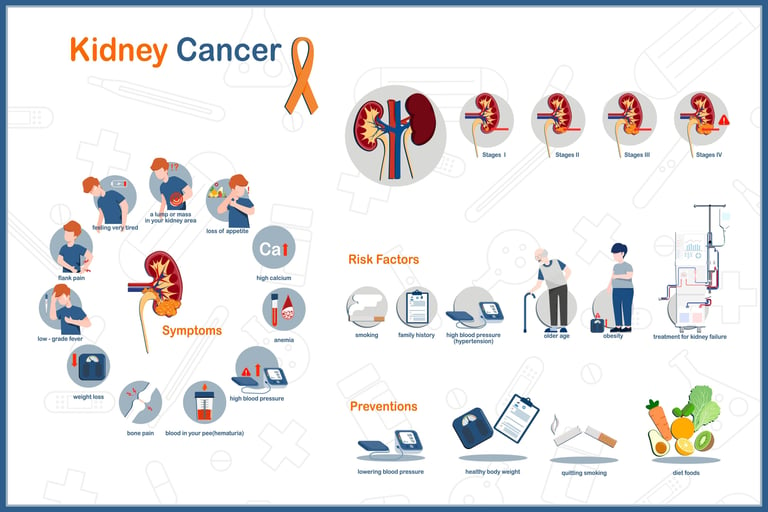
WHAT ARE THE RISK FACTORS?
There are many risk factors for developing kidney cancer. Some can be changed, while others depend on genetic or environmental factors.
The main known risk factors of kidney cancer are:
Smoking: The risk of kidney cancer is higher in smokers than in non-smokers, and quitting smoking can reduce this risk.
Obesity: Excess weight or obesity increases the risk of kidney cancer.
Hypertension: People with a history of hypertension have a higher risk of kidney cancer.
Family History of Cancer: In families with a history of kidney cancer, the risk may be higher.
Certain Medications and Medical Conditions: Long-term use of painkillers or some chronic kidney diseases may increase the risk of kidney cancer.
Age: Kidney cancer usually occurs in people over the age of 60.
Gender: Men have a higher risk of kidney cancer than women.
Genetic and Hereditary Syndromes: Von Hippel-Lindau disease, Birt-Hogg-Dubé syndrome, and some other genetic conditions may increase the risk of kidney cancer.
Environmental Exposures: Exposure to asbestos, cadmium and some organic solvents may also increase the risk.
Kidney cancer risk may depend on a combination of these factors. Lifestyle changes, especially quitting smoking and maintaining a healthy body weight, may be important in reducing risk. In addition, regular health checks for individuals at high risk can increase the chances of early diagnosis and treatment.
Image 1: Kidney cancer can cause complaints such as weight loss, pain and fever.
HOW IT OCCURS
Although the mechanisms of development of kidney cancer are complex and not fully resolved, they are associated with a combination of genetic mutations and environmental influences. Kidney cancer usually begins in the small ducts of the kidney and grows and proliferates uncontrollably due to mutations in the DNA of the cells there. These genetic changes disrupt the normal growth and death processes of cells, leading to the accumulation of abnormal cells and tumor formation. Especially in renal cell carcinoma (RCC), changes in the von Hippel-Lindau (VHL) gene play an important role. Environmental factors, especially risk factors such as smoking, exposure to chemicals, and obesity, can trigger the development of kidney cancer. Additionally, chronic kidney diseases such as inflammation and hypertension can also increase the risk of developing cancer. The interaction of these factors plays an important role in the development of kidney cancer and contributes to the diverse biological behaviors of cancer. Therefore, research on kidney cancer is aimed at better understanding the disease and developing effective treatment methods.
WHAT ARE THE SYMPTOMS?
Kidney cancer can often be asymptomatic in its initial stages, but as the cancer progresses, various symptoms may appear.
Common symptoms of kidney cancer:
Hematuria (Bloody Urine): One of the most common symptoms is blood in the urine. Blood can make urine pink, red, or cola-colored.
Waist or Side Pain: There may be persistent pain on the side where the kidney is located, usually in the lower back.
Weight Loss: Unexplained and unintentional weight loss may occur.
Tiredness: There may be persistent fatigue or weakness.
Fever: There may be unexplained intermittent fever.
Swelling or Mass: There may be swelling or a palpable mass in the abdomen or kidney area.
Anemia: There may be symptoms of anemia such as weakness and pallor.
Night Sweats: Severe night sweats may occur.
Anorexia: There is a general loss of appetite.
These symptoms do not always indicate kidney cancer and may indicate other health problems. However, it is important for people experiencing such symptoms to see a doctor for medical evaluation. Early diagnosis plays a very important role in kidney cancer treatment.
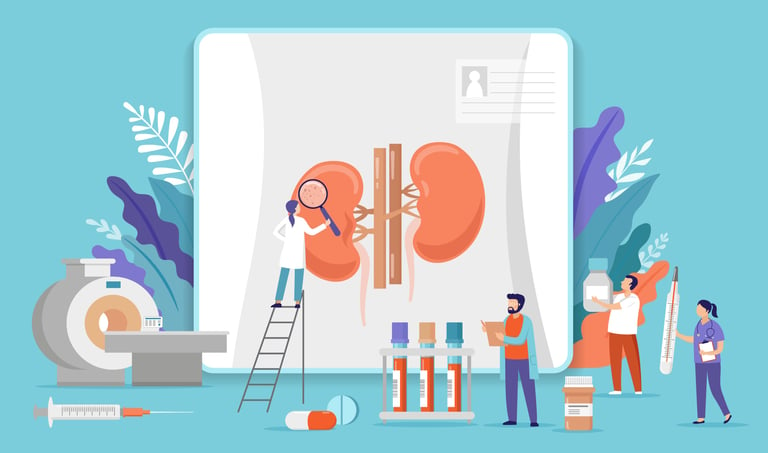
HOW IS IT DIAGNOSED?
Kidney cancer is usually diagnosed using a variety of diagnostic tests and procedures. The process typically begins with the patient's symptoms and medical history. During a physical examination, the doctor may look for a mass or swelling in the abdominal area. The most common and effective diagnostic tools include imaging tests; Methods such as ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI) are used to detect abnormalities, masses or tumors in the kidneys. These imaging tests are critical to determine the size, location, and possible spread of the tumor. Sometimes it may be necessary to take a tissue sample from the kidney to make a more definitive diagnosis or to determine the type of cancer; This procedure is called a biopsy and is performed by examining the sample under a microscope. Additionally, blood tests and urine analysis are performed to evaluate kidney function and general health status. This comprehensive evaluation ensures the correct diagnosis and helps determine the appropriate treatment plan. Early diagnosis is critical in treating kidney cancer because early-stage cancers can often be treated more successfully.
WHAT ARE THE PATHOLOGICAL TYPES?
Kidney cancer is divided into several pathological types, and each type is classified according to the cell type from which the cancer originates and its microscopic features.
The most common pathological types of kidney cancer:
Renal Cell Carcinoma (RCC): It is the most common type of kidney cancer and usually arises from tubular epithelial cells in the cortical region of the kidney.
RCC has specific subtypes:
Clear Cell RCC: It is the most common type of RCC and usually follows an aggressive course.
Papillae RCC: It is the second most common type and is divided into two subtypes: Type 1 and Type 2.
Chromophobe RCC : It is less common and generally has a better prognosis.
Medullary Carcinoma: It is a type of RCC that is very rare and generally has a poor prognosis.
Collecting Duct Carcinoma (Bellini Duct Carcinoma): It is a rare but usually aggressive type of RCC.
Urothelial Carcinoma (Upper Urinary System Cancer): This type can develop in the pelvis (renal pool) and ureters of the kidney and has features similar to bladder cancer.
Wilms Tumor (Nephroblastoma): It is a type of kidney cancer seen in children and usually responds well to treatment.
Carcinomas with Sarcomatoid Differentiation: This type is an aggressive variant of RCC with sarcomatoid features.
The pathological type of kidney cancer plays an important role in determining treatment options and the patient's prognosis. Each species differs in biological behavior and response to treatment. Therefore, accurate pathological diagnosis is critical for determining appropriate treatment strategies. In kidney cancer, especially renal cell carcinoma (RCC), some molecular receptors and biological markers are of great importance for determining treatment and monitoring the course of the disease. The most important are Vascular Endothelial Growth Factor (VEGF) receptors; VEGF encourages tumors to form blood vessels and plays a critical role in the growth and spread of kidney cancer. Drugs targeting VEGF receptors are used in the treatment of RCC. The Mammalian Target of Rapamycin (mTOR) pathway may also be hyperactive in RCC, and mTOR inhibitors are used in the treatment of advanced RCC. Additionally, immunotherapy targets Programmed Death-1 (PD-1) and Programmed Death Ligand-1 (PD-L1) receptors offer new and effective options for RCC treatment. Besides these receptors, Epidermal Growth Factor Receptors (EGFR) and Carbonic Anhydrase IX (CAIX) may also be important in some cases of RCC. Understanding and evaluating these molecular factors play an important role in the diagnosis, treatment, and monitoring of disease progression of RCC, which helps develop personalized treatment strategies.
Image 2: In people with suspected kidney cancer, a biopsy may be performed after CT or MRI evaluation.
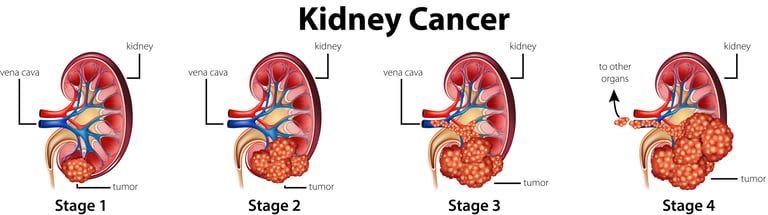
HOW IS TUMOR STAGING DONE IN CANCER?
Tumor staging in kidney cancer is a process used to determine the size and spread of the cancer. Staging is critical for treatment planning and prognosis prediction. It is usually based on the TNM (Tumor, Node, Metastasis) system and includes the following criteria:
T (Tumor): It evaluates the size and local spread of the tumor in the kidney.
T1: The tumor is smaller than 7 cm and is only inside the kidney.
T2: The tumor is larger than 7 cm but is still only inside the kidney.
T3: The tumor has spread to the main vessels of the kidney or surrounding tissues, but does not involve nearby glands.
T4: The tumor has spread beyond the kidney glands and into surrounding tissues.
N (Node): It indicates spread to regional lymph nodes.
N0: There is no cancer in the lymph nodes.
N1: There is cancer in the regional lymph nodes.
M (Metastasis): Determines the presence of distant metastasis.
M0: There is no distant metastasis.
M1: There is distant metastasis.
G (Grade): It indicates the grade of the tumor or how aggressive it is. Fuhrman grading is often used for kidney cancer, with grade 1 representing the least aggressive tumor and grade 4 representing the most aggressive tumor.
Kidney cancer staging plays an important role in predicting treatments for the disease and overall patient survival rates. While early-stage kidney cancer can usually be treated with surgery, systemic treatments or palliative care may be preferred in advanced-stage cancers. Staging is a key factor to guide the patient's treatment process and follow-up.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Treatment of kidney cancer varies depending on the stage of the cancer. Treatment methods vary for each stage, and factors such as the person's general health condition, age and response to treatment also play a role in treatment choices.
General treatment approaches according to the stages of kidney cancer:
Stage I and II (Localized Kidney Cancer)
Surgery: The most common treatment method is to remove all of the kidney (radical nephrectomy) or part of it (partial nephrectomy).
Ablative Treatments: Methods such as radiofrequency ablation or cryoablation may be preferred for small tumors.
Stage III (Regional Spread)
Surgery: Removal of the kidney and affected lymph nodes.
Systemic Treatments: After surgery or in cases where surgery cannot be performed, targeted treatments or immunotherapy can be used.
Stage IV (Metastatic Kidney Cancer)
Targeted Therapies: In advanced stages of renal cell carcinoma, drugs such as VEGF inhibitors (e.g., sunitinib, pazopanib) and mTOR inhibitors (e.g., temsirolimus) are used.
Immunotherapy: Immunotherapeutic agents such as PD-1/PD-L1 inhibitors (e.g., nivolumab).
Surgery: Sometimes may be performed to remove metastases or control symptoms.
Palliative Care: Supportive treatments to control pain and improve quality of life.
Kidney cancer treatment requires a personalized approach for each patient. The treatment plan is personalized based on the type of tumor, the patient's overall health and personal preferences. In addition, regular follow-up and evaluation during the treatment process is important to monitor the response to treatment and adjust the treatment if necessary. While early-stage kidney cancer is usually treatable, treatment for advanced-stage cancers can be more difficult and is usually focused on controlling the progression of the disease.
Image 3: The main treatment method for kidney cancer is surgery. Smart drug treatments are used in end-stage patients.
WHAT ARE THE SYSTEMIC DRUGS USED IN TREATMENT?
Kidney cancer, especially in the treatment of renal cell carcinoma (RCC), generally does not respond well to chemotherapy, so treatment is dominated by targeted therapies and immunotherapy.
Various treatment methods and drugs used in kidney cancer:
Targeted Therapies (Smart Drugs): Tyrosine kinase inhibitors (Sunitinib, Pazopanib, Sorafenib, Axitinib), mTOR Inhibitors (Temsirolimus, Everolimus), VEGF Inhibitors (Bevacizumab) can be used.
Immunotherapies: PD-1/PD-L1 Inhibitors (Nivolumab, Pembrolizumab, Avelumab) and CTLA-4 Inhibitors (Ipilimumab, sometimes used in combination with PD-1/PD-L1 inhibitors) may be used
Chemotherapy: RCC does not usually respond to chemotherapy and is therefore not used as a standard treatment method.
Treatment options for kidney cancer are determined according to the patient's general health condition, the characteristics of the cancer and its stage. The treatment process aims to maximize the patient's quality of life and control the progression of the disease. The treatment plan is reviewed regularly and adjustments are made if necessary.
HOW SHOULD FOLLOW-UP BE DONE AFTER RECOVERY?
Follow-up after recovery from kidney cancer is vital to ensure early intervention against the possibility of disease recurrence and to monitor the patient's long-term health. Follow-up usually begins after completion of surgery or other treatment methods and may last for several years. This process includes regular physical exams, blood tests (kidney function tests and tumor markers if necessary), and periodic imaging tests (for example, computed tomography (CT) or magnetic resonance imaging (MRI). During the first few years, these check-ups are usually done more frequently. because the risk of relapse is higher during this period. Frequency of follow-up may be reduced for patients who show no symptoms over time. It is important for patients to contact their healthcare provider immediately with any new symptoms or concerns. Regular follow-ups are also performed to manage long-term side effects of treatment and optimize overall health. Taking a proactive approach to potential post-complications of kidney cancer treatment helps protect the patient's overall health and maximize quality of life.