Cervical Cancer
21.03.2025
CERVICAL CANCER DIAGNOSIS AND TREATMENT
Cervical cancer is a type of cancer that originates from the cervix, also known as the cervix. The cervix, an important part of the female reproductive system, forms the lower part of the uterus and opens into the vagina. Cervical cancer is most often associated with human papillomavirus (HPV) infection and is a leading cause of cancer death among women worldwide. It usually does not cause symptoms in the early stages, but as it progresses, symptoms such as vaginal bleeding, pelvic pain and pain during intercourse may occur. Cervical cancer is important because it can be diagnosed early and treated effectively with regular screening tests (Pap smear and HPV test). Additionally, the HPV vaccine is considered an important preventative of this type of cancer and is used to reduce the risk of this cancer in young women and men. Therefore, regular screenings, raising awareness about the HPV vaccine and ensuring early diagnosis are critical in the fight against cervical cancer. These measures are of great value to prevent the spread of the disease and increase the success of treatment.
WHAT ARE THE RISK FACTORS?
Cervical cancer is associated with various risk factors. These factors may increase a woman's chance of developing cervical cancer. Known risk factors of cervical cancer include:
Human Papillomavirus (HPV) Infection: The most common cause of cervical cancer is chronic infections, especially those caused by high-risk HPV types (e.g. HPV 16 and 18).
Multiple Sexual Partners or Early Sexual Activity: Multiple sexual partners or sexual activity at an early age increases the risk of HPV infection.
Weak Immune System: Conditions that weaken the immune system, such as HIV infection, increase the risk of HPV infections and therefore cervical cancer.
Smoking: Smoking increases the risk of cervical cancer, as chemicals in cigarette smoke can cause changes in the cervix.
Long Term Birth Control Pill Use: Long-term (more than 5 years) use of birth control pills may increase a woman's risk of cervical cancer.
Multiple Births: Having more than one birth may also increase the risk, but this relationship is not fully understood.
Socio-Economic Factors: Low socioeconomic status, lack of access to regular health check-ups, and lack of preventative measures such as HPV vaccination may increase the risk of cervical cancer.
Family History of Cancer: Women with a family history of cervical cancer may be at higher risk.
Although each of these risk factors is not a definitive cause for developing cervical cancer, it may increase the risk. Therefore, regular screening and HPV vaccination play an important role in reducing the risk of cervical cancer. It is critical for women to understand their risk factors and have regular health checks in the early diagnosis and treatment of this type of cancer.
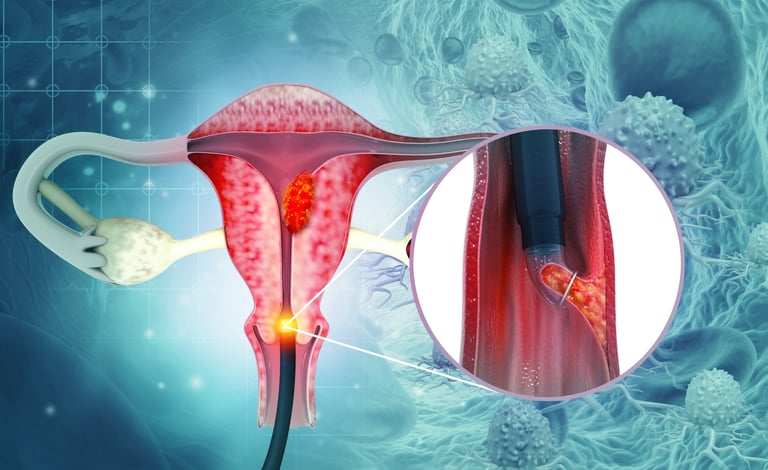
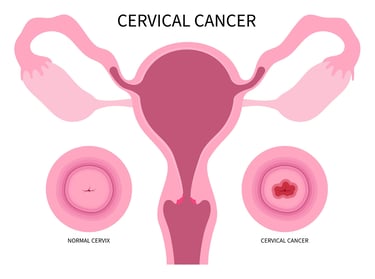
Image 1: Cervical cancer occurs at the end of the uterus.
HOW DOES IT OCCUR?
The main mechanism of cervical cancer development is chronic infections, usually caused by high-risk human papillomavirus (HPV) strains. HPV infects cervical cells and integrates into the DNA of these cells, disrupting the cells' normal growth and death patterns, causing them to turn into cancerous cells. This process usually takes years or even decades, and most HPV infections go away on their own, but some can turn into cancer. HPV damage to cells, especially through abnormal activation of E6 and E7 oncoproteins, disrupts the cell's DNA repair mechanisms and causes uncontrolled cell division. This can lead to the development of precancerous lesions in the cervix (e.g. cervical intraepithelial neoplasia - CIN) and eventually cervical cancer. Smoking, a weak immune system, and other environmental factors can accelerate or worsen this process. Understanding the development of cervical cancer is important for early diagnosis and development of effective treatment strategies, so regular screenings and HPV vaccination play a critical role in combating this type of cancer.
WHAT ARE THE SYMPTOMS?
Cervical cancer often has no symptoms in the early stages, which can make it difficult to diagnose. However, some symptoms may occur in later stages. Common findings of cervical cancer include:
Abnormal Vaginal Bleeding: The most common symptom is abnormal bleeding that occurs between menstrual periods, after sexual intercourse, or in the postmenopausal period.
Vaginal discharge: Abnormal, sometimes foul-smelling or bloody vaginal discharge may be observed.
Pelvic Pain: Pelvic pain or discomfort is common, especially during sexual intercourse.
Irregular Menstrual Bleeding: There may be changes in menstrual cycles or unexpected bleeding.
Changes in Urine or Stool: In advanced stages, the urinary tract or rectum may be affected, leading to pain during urination or changes in defecation habits.
Abdominal or Back Pain: In advanced stages, pain may be felt in the abdomen or lower back.
These symptoms may not be specific to cervical cancer and may be caused by other health problems. However, if you have any one or more of these symptoms, especially if they are persistent or severe, it is important to see a physician. Early diagnosis plays a critical role in successfully treating cervical cancer. Therefore, regular Pap smear tests and, if necessary, HPV tests play a key role in the early diagnosis of this type of cancer.
HOW IS IT DIAGNOSED?
Cervical cancer is diagnosed through a comprehensive process consisting of a series of steps. The first step is usually to further evaluate women who show abnormal Pap smear test results or symptoms of cervical cancer. Upon abnormal Pap smear findings, colposcopy is performed for a more definitive evaluation; This procedure uses a special microscope that provides a magnified image of the cervix. During colposcopy, biopsies may be taken from suspicious areas. These biopsy samples are examined under a microscope to detect the presence of cancer cells. Additionally, it may be necessary to examine samples taken by curettage from within the cervical canal. When necessary, imaging tests such as magnetic resonance imaging (MRI), computed tomography (CT) or positron emission tomography (PET) may be used to evaluate the spread and stage of the cancer. During the diagnosis phase, HPV DNA testing can help determine the type of infection and the risk of developing cancer. These steps are used together to accurately determine the presence and stage of cervical cancer and are critical in determining the patient's treatment plan. The diagnostic process is personalized according to each patient's condition and is of fundamental importance for the effectiveness of treatment strategies.
WHAT ARE THE PATHOLOGICAL TYPES?
Cervical cancer is generally classified into two main pathological types. These types are distinguished according to the cellular structure of the cancer visible under the microscope, and each involves different treatment approaches and prognoses. The main pathological types of cervical cancer are:
Squamous Cell Carcinoma: This type, which constitutes the majority of cervical cancers, arises from squamous (flat) cells in the outer layer of the cervix. This type of cancer usually grows slowly and is most often associated with HPV infection.
Adenocarcinoma:This less common type arises from the mucus-secreting gland cells of the cervix. Adenocarcinomas may behave differently than squamous cell carcinomas and sometimes be more aggressive.
Other rare types include adenosquamous carcinoma and other less common variants. These rare types may display both glandular and squamous cell characteristics and require different treatment strategies. In the diagnostic process, determining the pathological type plays an important role in evaluating the patient's treatment plan and prognosis. Pathological type is determined by microscopic examination of biopsy samples, and this information provides important clues about the cancer's potential to spread and its response to treatment. The biological behavior of each type, its response to treatment, and the patient's general health condition are taken into account in treatment planning.
The specific receptors or molecular markers that should be focused on when determining treatment options in cervical cancer are less clear than in other types of cancer. The main factor in the treatment of cervical cancer is primarily the stage of the disease and, in general, the presence of Human Papillomavirus (HPV) infection. The role of high-risk types of HPV (especially HPV 16 and 18) in the development of cervical cancer is critical in determining treatment approaches. Additionally, the presence of p16ink4a protein can be considered as an indicator of HPV-related lesions and may be helpful in determining diagnosis and treatment strategies in some cases. Apart from this, specific hormonal receptors or other molecular targets do not play a decisive role in treatment decisions in cervical cancer. The use of immunotherapies may be considered in patients with positive PD-L1 levels.
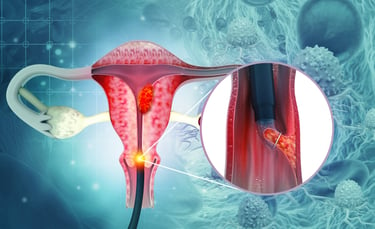
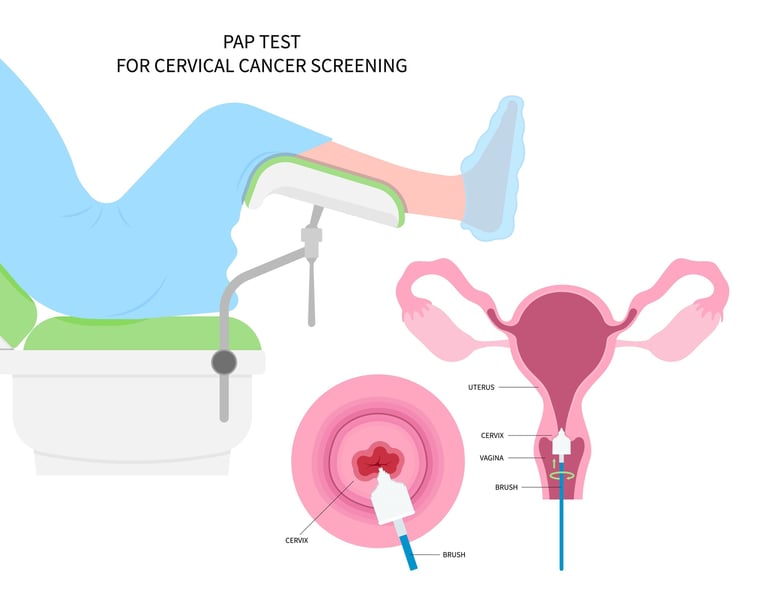
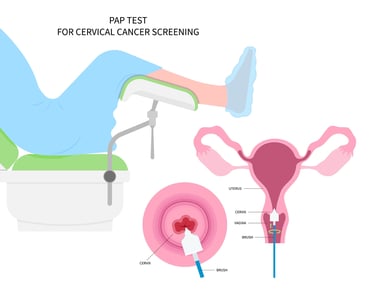
Image 2: Early diagnosis and treatment of cervical cancer is possible thanks to the screening method with smear test and HPV DNA test.
HOW IS TUMOR STAGING DONE?
Tumor staging in cervical cancer is a method used to determine how far the cancer has progressed and whether it has spread to other parts of the body. Staging has an important role in determining the treatment plan and prognosis. The most widely used staging system for cervical cancer is the system developed by the International Federation of Gynecological and Obstetrics (FIGO). This system is based on the anatomical spread of cancer and is classified as follows:
Stage I: Cancer is found only in the cervix.
Stage IA: There is microscopic cancer (very small tumor).
Stage IB: There is a visible or larger tumor.
Stage II:The cancer has spread beyond the cervix but has not reached the pelvic wall or lower third of the vagina.
Stage IIA: It has spread to the upper two-thirds of the vagina.
Stage IIB: It has spread to the parameters (lateral tissues of the cervix).
Stage III: The cancer has spread to the pelvic wall or lower third of the vagina, or has led to hydronephrosis, or silent kidney, which affects the function of the kidneys.
Stage IIIA: It has spread to the lower third of the vagina.
Stage IIIB: It has spread to the pelvic wall or hydronephrosis/silent kidney has occurred.
Stage IIIC: There is spread to lymph nodes.
Stage IV:The cancer has spread beyond the pelvis.
Stage IVA: It has spread to the bladder or rectum.
Stage IVB: Distant metastases (e.g. lungs, liver) are present.
This staging is done based on the results of a physical examination, imaging tests (e.g., MRI, CT, PET scans), and biopsy if necessary. Staging is critical to understanding the extent of cancer spread and determining the most appropriate treatment strategy. Each stage shows different characteristics that indicate the spread and severity of cancer, and treatment approaches are determined accordingly.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Cervical cancer treatment varies depending on the stage of the cancer. Treatment is planned by taking into account how far the cancer has spread, the patient's general health condition and personal preferences. Below, general treatment methods are summarized according to the stages of cervical cancer:
Stage I:
Early Stage I: Early stage cervical cancer is usually treated with surgery, which may be conization or radical hysterectomy (removal of the uterus).
Advanced Stage I: For patients with larger tumors or high-risk factors, a combination of radiotherapy or chemotherapy may be recommended after surgery.
Stage II:
Radiotherapy and Chemotherapy: At this stage, cancer is mostly treated with a combination of radiotherapy and chemotherapy. Treatment aims to shrink the cancer and control its spread.
Stage III:
Radiotherapy and Chemotherapy: A combination of pelvic radiotherapy and chemotherapy is aimed at controlling the spread of cancer and relieving symptoms.
Stage IV (Cancer Has Spread Beyond the Pelvis):
Palliative Treatment: Treatment for Stage IV cervical cancer is usually palliative, focusing on relieving the patient's symptoms and improving their quality of life. Radiotherapy, chemotherapy or other symptomatic treatments may be given.
Targeted Therapies and Immunotherapy: In some cases, targeted therapies or immunotherapy options may also be considered for patients with advanced or recurrent cervical cancer.
In every treatment situation, management of side effects, supportive care, and treatment planning according to patient needs are important. Treatment options are personalized based on the characteristics of the cancer, the patient's general health status and preferences. In the treatment of cervical cancer, constantly developing new treatment methods and clinical research are also taken into account.
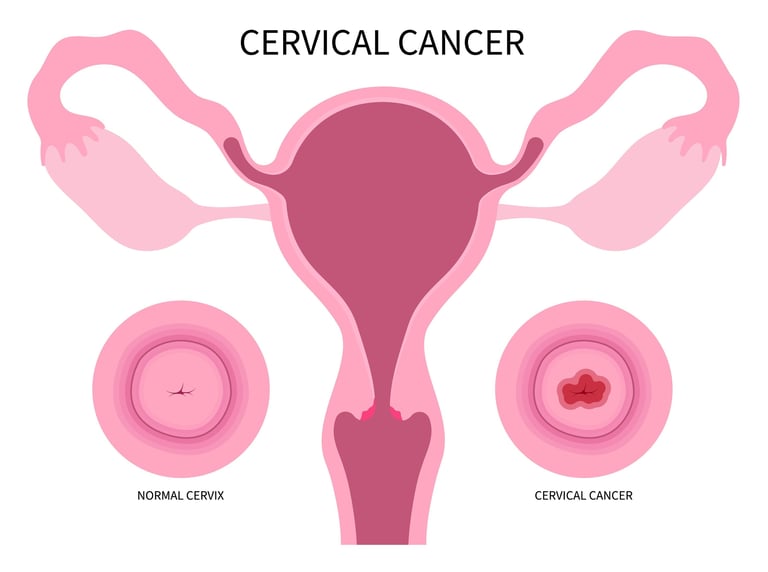
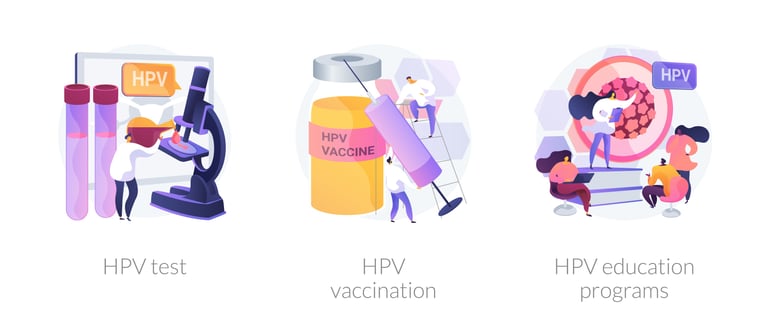
Image 3: The most common cause of cervical cancer is HPV infection. HPV vaccination should be given to children between the ages of 9 and 26.

WHAT ARE THE DRUGS USED IN TREATMENT?
There are various chemotherapy drugs, targeted therapies and immunotherapy options used in the treatment of cervical cancer. Some treatment methods used in cervical cancer:
Chemotherapy Drugs:
Cisplatin: It is the most commonly used chemotherapy drug in cervical cancer.
Carboplatin: It has a similar mechanism of action as cisplatin.
Paclitaxel: Stops cell division by inhibiting microtubule dynamics.
Topotecan: It is a topoisomerase I inhibitor.
5-Fluorouracil (5-FU): It is an antimetabolite that blocks DNA and RNA synthesis.
Gemcitabine: It is an antimetabolite that inhibits DNA synthesis.
Targeted Therapies and Immunotherapies:
Bevacizumab: It is an angiogenesis inhibitor and prevents cancer cells from forming blood vessels.
Pembrolizumab: It has an immunotherapeutic effect through the PD-1 pathway and is used especially in advanced stage or metastatic cervical cancer.
Nivolumab: Another PD-1 inhibitor and used similarly to pembrolizumab.
These treatment methods can be used alone or in combination, depending on the stage of the cancer, its spread, and the patient's general health condition. Treatment planning is specific to each patient and treatment options are made taking into account potential side effects and patient preferences. In the treatment of cervical cancer, new treatment options and clinical research are ongoing and treatment protocols are constantly evolving.
HOW SHOULD FOLLOW-UP BE CARRIED OUT AFTER RECOVERY?
Following cervical cancer treatment, it is important for patients to continue regular follow-up and check-up examinations. Generally, the follow-up schedule is determined depending on the patient's specific condition after surgery or radiotherapy and their response to treatment. Follow-up examinations are performed to evaluate the risk of cancer recurrence and to detect possible complications early. In these examinations, physical examination, smear test, HPV screening, blood tests and, if necessary, imaging methods may be used. Physicians will consider personal medical history, treatment history, and risk factors when determining a patient's follow-up plan. Cervical cancer patients should monitor their health closely by following the follow-up plan recommended by their doctor.