Brain Cancer
21.03.2024
BRAIN TUMOR DIAGNOSIS AND TREATMENT


A brain tumor is a condition caused by the uncontrolled proliferation of abnormal cells in the brain. These tumors can be benign or malignant. Benign tumors generally grow slower, do not spread to surrounding tissues, and are less likely to recur when treated. Malignant tumors, on the other hand, grow more aggressively and can spread to surrounding tissues. The importance of brain tumors lies in the fact that they affect a vital organ such as the brain and have the potential to spread to other parts of the body. Symptoms may vary depending on the location and size of the tumor and can lead to serious health problems such as headaches, visual disturbances, memory problems, personality changes and seizures. Early diagnosis and appropriate treatment can significantly improve the patient's survival rate and quality of life. Therefore, it is vital that people showing symptoms of brain tumors seek medical help without delay.
WHAT ARE THE RISK FACTORS?
Various risk factors for brain tumor formation have been identified. However, it is important to remember that the presence of these factors does not always lead to a brain tumor.
Some common risk factors associated with brain tumor:
Genetic Factors: Some genetic disorders and syndromes may increase the risk of brain tumors. For example, conditions such as neurofibromatosis, von Hippel-Lindau disease or Li-Fraumeni syndrome.
Family History: Close family members with a brain tumor may increase the risk, but this is not very common.
Age: Brain tumors can occur at any age, but some types are more common in certain age groups. For example, gliomas usually occur in adults, while medulloblastomas are more common in childhood.
Exposure to Radiation: Exposure to ionizing radiation, especially at high doses (for example, in people who have had radiation therapy), may increase the risk of brain tumors.
Environmental Factors: Some studies have suggested that long-term exposure to certain chemicals and toxins may increase the risk of brain tumors, but the evidence is not clear.
Gender: Some types of brain tumors are more common in men, while others are more common in women.
Exposure to Electromagnetic Fields: Studies are still ongoing regarding exposure to electromagnetic fields from sources such as cell phones and power lines. There is currently no clear evidence as to whether such exposures increase the risk of brain tumors.
Each of these risk factors can have varying degrees of influence on brain tumor development, and many brain tumors can develop without any of these risk factors.
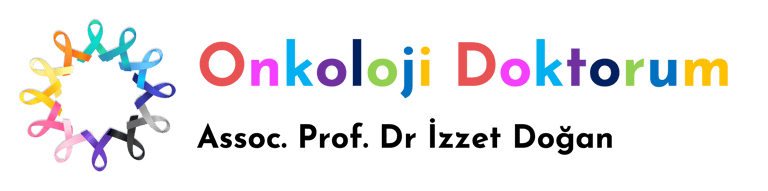
Image 1: Complaints such as persistent headache, epileptic seizures, nausea and vomiting may occur in brain tumors.
HOW IT OCCURS ?
The mechanisms of brain tumor development are quite complex and are often associated with a combination of genetic changes and environmental influences. Normally, the division and death of body cells is carefully regulated. However, genetic mutations in this regulatory process can cause cells to divide uncontrollably and fail to die, leading to tumor formation. Brain tumors can arise from different types of brain tissue, and each type of tumor has unique characteristics and behaviors. For example, astrocytomas that arise from astrocytes (supporting cells in the brain and spinal cord) and oligodendrogliomas that arise from oligodendroglial cells. Genetic changes, defects in the correction of DNA damage, malfunctions in cell cycle control mechanisms and disruptions in programmed cell death (apoptosis) processes play a role in the development of brain tumors. Additionally, external factors such as environmental factors and lifestyle choices may also play a role in triggering these genetic changes. This complex interaction contributes to the diversity of brain tumors and their different responses to treatment.
WHAT ARE THE SYMPTOMS?
Symptoms of a brain tumor may vary depending on the size, type and location of the tumor in the brain. But in general, some common symptoms are:
Headache: Headaches that are especially severe in the morning and worsen over time are a common symptom of a brain tumor.
Seizures: Seizures can occur in people with brain tumors, even in adults with no previous history of seizures.
Personality or Behavior Changes: Memory problems, confusion, difficulty concentrating or personality changes are among the symptoms of a brain tumor.
Vision and Hearing Problems: Vision or hearing problems such as blurred vision, double vision, hearing loss or tinnitus (ringing in the ears) may occur.
Speech Difficulties: There may be difficulty in speaking or incomprehensible speech.
Movement and Coordination Disorders: Numbness or tingling in the hands and feet, loss of coordination, imbalance, or difficulty walking may occur.
Muscle Weakness or Paralysis: Loss of strength or paralysis on one side of the body may occur.
Nausea and Vomiting: Nausea and vomiting, especially in the mornings and accompanied by headache, may occur.
These symptoms do not always indicate the presence of a brain tumor and may be caused by other health problems. However, a person experiencing any of the above symptoms should consult a physician for a definitive diagnosis and necessary treatment. It is important to seek medical help, especially if these symptoms occur more than once and continuously.
HOW IS IT DIAGNOSED?
Brain tumor diagnosis is made using various diagnostic tools and procedures. The first step is usually a detailed medical history of the patient and a physical neurological examination. This examination evaluates functions related to the brain and nervous system, such as reflexes, muscle strength, coordination, sensory ability and mental status. When symptoms and examination findings suggest a brain tumor, more detailed imaging tests are performed. These include magnetic resonance imaging (MRI) and computed tomography (CT) scans. MRI provides detailed images of brain tissue and is extremely useful in determining the presence, size, and location of a tumor in the brain. In some cases, other advanced imaging techniques such as positron emission tomography (PET) scanning or magnetic resonance spectroscopy (MRS) may also be used to better understand the characteristics of the tumor and determine the most appropriate treatment plan. If a tumor is suspected, a surgical biopsy may be performed to make a definitive diagnosis and determine the type of tumor. In this procedure, a small tissue sample is removed from the tumor and examined under a microscope. All of these diagnostic methods are used together to determine the presence, type, size and spread of the brain tumor, and this information is used to develop the most appropriate treatment strategy for the patient.
WHAT ARE THE PATHOLOGICAL TYPES?
Brain tumors are divided into many different types according to the cell type they originate from and their histopathological features.
Some of the most common pathological types of brain tumors are:
Gliomas: This group includes tumors arising from glial cells in the brain and spinal cord. Gliomas are divided into more specific subtypes:
Astrocytomas: Originate from astrocyte cells and usually occur in adults.
Oligodendrogliomas: They develop from oligodendrocyte cells and are usually located in the brain cortex (cortex).
Ependymomas: Originate from ependymal cells and are usually found in the spinal cord or brain ventricles.
Glioblastoma Multiforme (GBM): The most aggressive type of glioma and is generally characterized by rapid growth and poor prognosis.
Meningiomas: They are generally benign tumors arising from the meninges (membranes covering the brain).
Schwannoma: It develops from Schwann cells, which are nerve sheath cells. It is usually benign and is often found around the auditory nerve.
Pituitary Adenomas: They are generally benign tumors that develop in the pituitary gland and can cause hormonal imbalances.
Medulloblastomas: It is an aggressive and malignant tumor that is more common in children. These tumors develop in the cerebellum (small brain).
Craniopharyngiomas: These are generally benign tumors that develop near the brainstem and pituitary gland.
Primary Central Nervous System Lymphomas: It is a type of lymphoma that develops in the brain or spinal cord and is usually malignant.
Pineal Region Tumors: Tumors that develop in the pineal gland and are usually seen in children and young adults.
These are the most common pathological types of brain tumors, but these tumors can be very diverse and complex, and rarer types of tumors also exist. Each tumor type has different clinical features, treatment responses and prognoses. Therefore, detailed pathological examination is required for definitive diagnosis and appropriate treatment. In treatment planning and prognosis evaluation of brain tumors, it is vital to determine the molecular and genetic characteristics of the tumor. In this context, IDH1 and IDH2 gene mutations are considered important prognostic markers, especially for gliomas; Tumors with these mutations generally indicate a better prognosis. 1p/19q codeletion is a genetic abnormality seen in oligodendrogliomas and is generally associated with a more favorable prognosis and better response to chemotherapy. In glioblastomas, the presence of MGMT (O6-methylguanine-DNA methyltransferase) promoter methylation may imply better response to certain chemotherapy agents. PD-L1 (Programmed cell death ligand 1) expression is important for response to immunotherapy and is considered an important treatment target in some brain metastases. These molecular and genetic markers play critical roles in understanding tumor biological behavior, response to treatment, and patient prognosis. This information contributes significantly to the development of personalized treatment approaches and the discovery of new therapeutic strategies in brain tumor treatment. In modern brain tumor management, the importance of these molecular and genetic tests is increasing, allowing a better understanding of the tumor and the creation of effective treatment plans.
Image 2: Brain tumor diagnosis is made with CT and MRI.


HOW IS TUMOR STAGING DONE?
Tumor staging in brain tumors is performed to determine characteristics of the tumor such as its size, degree of spread and aggressiveness. However, staging of brain tumors differs from the traditional TNM (Tumor, Nodules, Metastasis) classification used for other types of cancer. Staging of brain tumors is generally based on the grading system established by the World Health Organization (WHO). This system makes a grade according to the histological features of the tumor and the degree of malignancy:
Grade I (Low Grade): These tumors are generally benign, slow-growing and limited to surrounding tissues. They can be completely removed with surgery and are unlikely to recur.
Grade II: These tumors are also slow-growing, but slightly more aggressive than Grade I tumors. They can still be completely removed with surgery, but they have a higher risk of recurrence and malignancy.
Grade III (High Grade): These tumors grow aggressively and tend to spread into surrounding tissues. They are treated with surgery, radiotherapy and chemotherapy, but often have a high risk of recurrence.
Grade IV (Highest Grade): These tumors are very aggressive and fast-growing tumors. They spread rapidly to surrounding tissues and response to treatment is more difficult. Tumors such as glioblastoma multiforme (GBM) fall into this category.
This grading system is determined by microscopic examination of the tumor and is made by looking at factors such as the type of tumor, the degree of abnormality of the cells, the number of mitosis (cell division), the presence of necrosis (tissue death) and vascular (vessel) proliferation. This staging plays an important role in treatment planning and prognosis prediction. For example, higher grade (Grade III and IV) tumors often require more aggressive treatment and the prognosis may be worse. Therefore, accurate diagnosis and staging are critical in brain tumor treatment.
HOW IS TREATMENT DONE ACCORDING TO STAGES?
Treatment of brain tumors varies depending on the type, size, location, grade (stage) of the tumor and the patient's general health condition. Treatment options according to the stages of brain tumors are generally as follows:
Grade I and II (Low Grade Tumors):
Surgery: The first treatment option is usually to remove as much of the tumor as possible. In some cases, the tumor can be removed completely and surgery works best.
Radiotherapy: Used after surgery or if surgery is not possible. It may be used in some low-grade tumors to slow or stop the growth of the tumor.
Chemotherapy: Often considered as an adjunct to surgery and/or radiotherapy, especially if the tumor cannot be completely removed or has recurred.
Grade III and IV (High Grade Tumors):
Surgery: The aim is to remove as much tumor tissue as possible, but due to the aggressive nature of these tumors, complete removal may be difficult.
Radiotherapy: It is almost always administered after surgery. It plays a key role in the treatment of high-grade tumors.
Chemotherapy: Often used alone or with radiotherapy. Some medications are commonly used, especially in glioblastomas.
In all treatment options, a personalized treatment plan is created by taking into account the patient's health status, age, location of the tumor and other health conditions. Supportive care and rehabilitation are also important to manage side effects of treatment and improve quality of life. Brain tumor treatment usually requires a multidisciplinary approach and is carried out in collaboration with physicians from neurosurgery, oncology, radiation oncology and other oncology specialties. The most appropriate treatment plan for each patient is designed specifically according to the characteristics of the tumor and patient needs.
Image 3: Brain tumor treatment is primarily done with surgery. When surgery is not possible, radiotherapy and chemotherapy are applied.


WHAT ARE THE SYSTEMIC DRUGS USED IN TREATMENT?
Chemotherapy drugs, hormonal treatments, smart drugs and immunotherapies used in the treatment of brain tumors vary depending on the type and characteristics of the tumor.
Chemotherapy Drugs
Temozolomide: It is especially used in the treatment of high-grade gliomas such as glioblastoma and anaplastic astrocytoma.
Carmustine (BCNU) and Lomustine (CCNU): These nitrosoureas are used in the treatment of brain tumors.
Vincristine: Often used in combination with other chemotherapy drugs.
Platinum Based Drugs (Cisplatin, Carboplatin): Can be used for some brain tumors.
Smart Drug Therapies (Targeted Therapies)
Bevacizumab: It targets the vascular endothelial growth factor (VEGF) pathway and is used especially in the treatment of glioblastoma.
Erlotinib and Gefitinib: These are drugs that target the EGFR pathway.
Lapatinib: Targets the HER2/neu pathway and is being investigated for some brain tumors.
Immunotherapies
Nivolumab and Pembrolizumab: PD-1 pathway inhibitors are being investigated in the treatment of brain tumors.
Ipilimumab: CTLA-4 pathway inhibitor; In some cases, it is used for brain tumors.
Cancer Vaccines (e.g., DCVax-L, Rintega): Specialized treatments being investigated specifically for glioblastoma.
These drugs and treatment methods are selected based on the biological characteristics of the tumor, the patient's general health condition and previous responses to treatment. The development of treatment options continues constantly, and clinical studies enable the discovery of new and more effective treatment methods. As always, specific treatment options and combinations should be determined by the oncologist based on the type of tumor being treated and the individual situation of the patient.
HOW SHOULD FOLLOW-UP BE DONE AFTER RECOVERY?
Follow-up during the recovery period after brain tumor treatment is vital to reduce the risk of tumor recurrence and provide early intervention. Post-recovery follow-up usually includes regular neurological exams and imaging tests such as MRI. These examinations are performed to detect early signs of tumor return or new abnormalities. Patients usually undergo imaging tests frequently (e.g., every 3-6 months) during the first few years after treatment. Over time and as the patient's condition stabilizes, the frequency of these tests may be reduced. In addition, regular check-ups are performed to monitor patients' neurological functions, cognitive status and general health. During this period, patients are advised to contact their doctor immediately in case of any new symptoms or concerns. Physical and cognitive rehabilitation programs may also be important to improve quality of life and support functional recovery during the recovery process. Additionally, emotional and psychological support can be vital for patients and their families in the post-treatment period. Therefore, patients and their families are encouraged to utilize psychological counseling or support groups when necessary. Post-recovery follow-up requires a multidisciplinary approach, given the nature of the disease and the complexity of the treatment, and this process requires the patient to be in constant communication with neurosurgery, medical oncology and radiation oncology.